Burtom ‣ Technologies ‣ Magnetic Resonance Imaging 1.5 Tesla (MRI)
Language: 🇬🇧 English | 🇹🇷 Türkçe
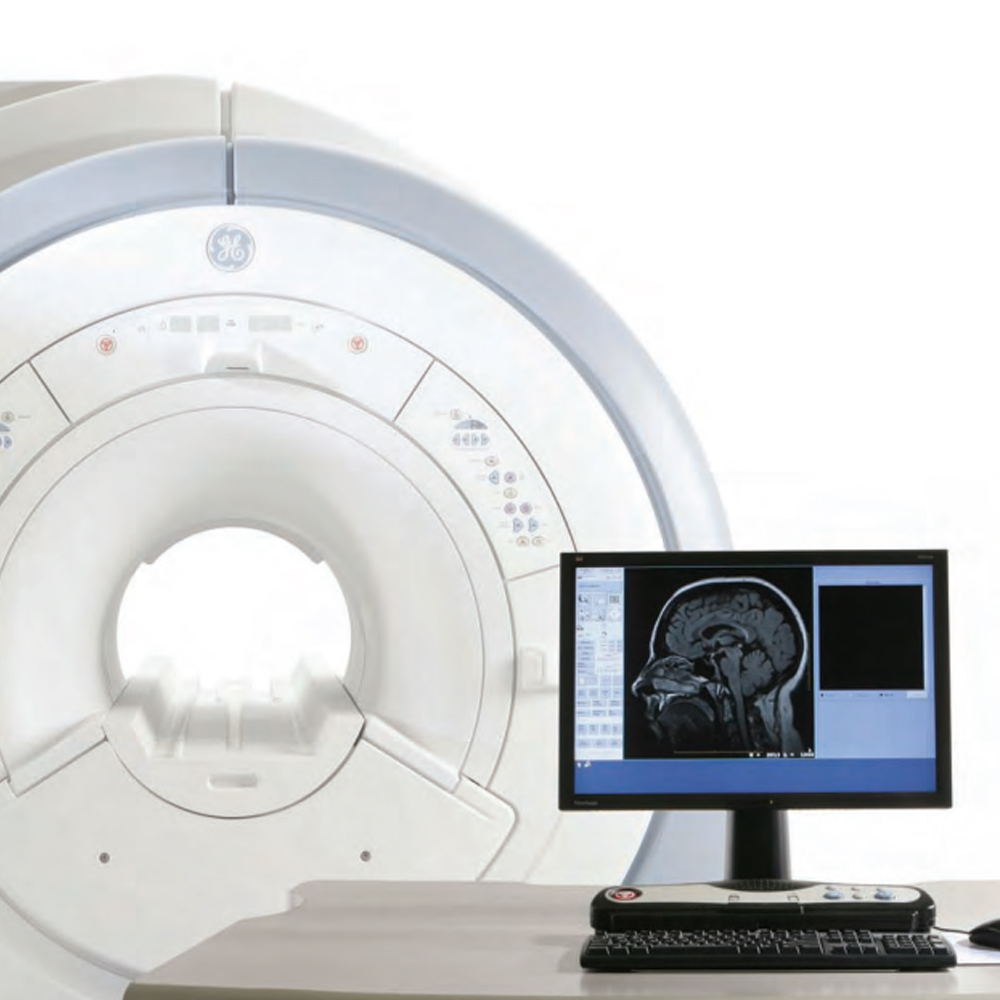
Magnetic Resonance Imaging 1.5 Tesla (MRI) Overview

 An overview of Magnetic Resonance Imaging (MRI) at 1.5 Tesla reveals a cutting-edge medical imaging technique that offers a detailed and comprehensive assessment of internal bodily structures and tissues. Operating on the principles of magnetic fields, radiofrequency pulses, and advanced computer processing, this state-of-the-art imaging modality generates highly detailed cross-sectional images of organs, tissues, and anatomical regions throughout the body. With its remarkable image resolution and versatility, 1.5 Tesla MRI plays a pivotal role in the diagnosis, evaluation, and monitoring of a wide range of medical conditions, including neurological disorders, musculoskeletal injuries, cardiovascular diseases, and oncological abnormalities. Its non-invasive nature and ability to capture intricate anatomical details make it an indispensable tool for healthcare professionals in delivering accurate diagnoses and formulating effective treatment plans tailored to each patient’s unique needs.
An overview of Magnetic Resonance Imaging (MRI) at 1.5 Tesla reveals a cutting-edge medical imaging technique that offers a detailed and comprehensive assessment of internal bodily structures and tissues. Operating on the principles of magnetic fields, radiofrequency pulses, and advanced computer processing, this state-of-the-art imaging modality generates highly detailed cross-sectional images of organs, tissues, and anatomical regions throughout the body. With its remarkable image resolution and versatility, 1.5 Tesla MRI plays a pivotal role in the diagnosis, evaluation, and monitoring of a wide range of medical conditions, including neurological disorders, musculoskeletal injuries, cardiovascular diseases, and oncological abnormalities. Its non-invasive nature and ability to capture intricate anatomical details make it an indispensable tool for healthcare professionals in delivering accurate diagnoses and formulating effective treatment plans tailored to each patient’s unique needs.
What is Magnetic Resonance Imaging (MRI) and How Does It Work?

Magnetic Resonance Imaging (MRI) is a non-invasive medical imaging technique used to visualize internal structures of the body in detail. It works by utilizing a powerful magnetic field, radiofrequency waves, and a computer to generate detailed images of organs, tissues, and other structures inside the body.
Here’s how MRI works:
Magnetic Field: The patient is placed inside a strong magnetic field produced by the MRI machine. This magnetic field aligns the hydrogen atoms within the body’s tissues.
Radiofrequency Pulse: Radiofrequency pulses are then applied to the body, causing the aligned hydrogen atoms to emit signals. These signals vary depending on the type of tissue they come from.
Signal Detection: The MRI machine detects these signals and processes them using advanced computer algorithms to create detailed images of the internal structures.
Image Formation: The signals are converted into cross-sectional images of the body, which can be viewed in different planes (such as axial, sagittal, and coronal) to provide a comprehensive view of the area being imaged.
By analyzing these images, healthcare professionals can diagnose and evaluate a wide range of conditions, including tumors, injuries, infections, and abnormalities in various organs and tissues throughout the body. MRI is particularly useful for imaging soft tissues like the brain, spinal cord, muscles, and joints, and it does not involve ionizing radiation, making it safe for most patients.
The basic principle of Magnetic Resonance Imaging (MRI) involves the interaction of magnetic fields and radio waves with the hydrogen atoms in the body’s tissues. Here’s an overview of the mechanism behind MRI:
Magnetic Field: The patient is placed inside a strong magnetic field generated by the MRI machine. This magnetic field causes the hydrogen nuclei (protons) in the body’s tissues to align themselves in a specific direction.
Radiofrequency Pulse: A brief burst of radiofrequency (RF) energy is then directed at the patient’s body. This RF pulse is applied at a frequency that matches the natural resonance frequency of the hydrogen nuclei in the magnetic field.
Absorption and Emission of Energy: When the RF pulse is applied, it causes the hydrogen nuclei to absorb energy and temporarily deviate from their aligned position. As the RF pulse is turned off, the hydrogen nuclei release this absorbed energy and return to their original alignment.
Signal Detection: As the hydrogen nuclei return to their original alignment, they emit radiofrequency signals. These signals are detected by specialized antennas in the MRI machine called radiofrequency coils.
Image Reconstruction: The detected signals are processed by a computer and used to generate detailed cross-sectional images of the body’s internal structures. By analyzing the signal intensity and distribution, healthcare professionals can visualize different tissues and organs in the body.
Overall, MRI relies on the principles of nuclear magnetic resonance (NMR) to create detailed images of the body’s anatomy. This non-invasive imaging technique is particularly valuable for visualizing soft tissues, such as the brain, spinal cord, muscles, and joints, and it plays a crucial role in diagnosing various medical conditions.
The patient experience during Magnetic Resonance Imaging (MRI) scanning can vary depending on individual preferences, the specific MRI procedure, and the patient’s medical condition. However, here is an overview of what patients can typically expect during an MRI scan:
Preparation: Before the MRI scan, patients may be asked to change into a hospital gown and remove any metal objects, such as jewelry, watches, and hairpins, as these can interfere with the magnetic field. Patients may also need to complete a screening questionnaire to ensure safety during the procedure.
Positioning: Patients are positioned on a motorized table that slides into the opening of the MRI machine. Depending on the area of the body being scanned, patients may need to lie flat on their back, stomach, or side. It’s essential to remain as still as possible during the scan to obtain clear images.
Noise: MRI machines generate loud knocking or tapping sounds during the scanning process, which can be unsettling for some patients. To minimize discomfort, patients are often provided with earplugs or headphones to reduce the noise level.
Communication: Patients are typically in constant communication with the MRI technologist or radiologist throughout the procedure. They may be able to communicate through an intercom system or hand signals to address any concerns or discomfort.
Comfort: MRI scans can take anywhere from 15 minutes to over an hour, depending on the complexity of the exam. Patients may experience discomfort from lying still for an extended period, especially if they have claustrophobia or chronic pain. Some MRI facilities offer comfort measures such as pillows, blankets, or music to help patients relax during the scan.
Safety: MRI is a safe and non-invasive imaging technique that does not use ionizing radiation. However, patients with certain medical implants or devices, such as pacemakers, cochlear implants, or metallic foreign bodies, may not be eligible for MRI scanning due to safety concerns.
Post-Scan: After the MRI scan is complete, patients are usually free to resume their normal activities. In some cases, patients may experience mild discomfort or dizziness immediately after the scan, but these symptoms typically resolve quickly.
Overall, while the MRI scanning process may be intimidating for some patients, healthcare providers strive to ensure a comfortable and safe experience by addressing patient concerns and providing necessary support throughout the procedure.
1.5 Tesla Magnetic Resonance Imaging (1.5T MRI)
1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) is a powerful medical imaging technique that utilizes a magnetic field with a strength of 1.5 Tesla to produce detailed images of the internal structures of the body. This imaging modality is widely used in clinical practice for its high resolution, excellent tissue contrast, and versatility in visualizing various anatomical regions and pathologies. By harnessing the principles of magnetic resonance, 1.5T MRI plays a crucial role in the diagnosis, treatment planning, and monitoring of a wide range of medical conditions, including neurological disorders, musculoskeletal injuries, cardiovascular diseases, and oncological abnormalities. Its non-invasive nature and ability to capture detailed anatomical information make it an invaluable tool in modern healthcare.
The characteristics and advantages of a 1.5 Tesla magnetic field in Magnetic Resonance Imaging (MRI) are significant factors that contribute to its widespread use and effectiveness in clinical practice. Here are some key characteristics and advantages:
High Signal-to-Noise Ratio: A 1.5 Tesla magnetic field provides a strong and uniform magnetic environment, resulting in a high signal-to-noise ratio (SNR) in MRI images. This high SNR improves image quality and enhances the ability to visualize fine anatomical structures and subtle pathologies.
Excellent Tissue Contrast: The 1.5 Tesla magnetic field generates excellent tissue contrast in MRI images, allowing for clear differentiation between different types of tissues based on their magnetic properties. This enables healthcare professionals to identify abnormalities and diagnose various medical conditions accurately.
Versatility: MRI scanners operating at 1.5 Tesla are versatile and can be used to image a wide range of anatomical regions and pathologies throughout the body. From neurological and musculoskeletal imaging to abdominal and cardiac imaging, 1.5T MRI offers comprehensive diagnostic capabilities.
Clinical Validation: 1.5 Tesla MRI systems have been extensively validated and used in clinical research and practice for decades. Their reliability, reproducibility, and established protocols make them a trusted imaging modality for healthcare providers worldwide.
Patient Comfort: Despite its strong magnetic field, 1.5T MRI scanners are designed with patient comfort in mind. The bore size of the scanner accommodates patients of various sizes, and advanced imaging techniques, such as parallel imaging and shorter scan times, help minimize patient discomfort during the examination.
Cost-Effectiveness: Compared to higher field strength MRI systems, such as 3 Tesla (3T) or higher, 1.5T MRI systems are often more cost-effective to purchase and operate while still providing excellent imaging capabilities. This makes them a preferred choice for many healthcare facilities.
Compatibility with Imaging Techniques: The 1.5 Tesla magnetic field is compatible with a wide range of advanced imaging techniques and sequences, including diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI), and functional MRI (fMRI). These techniques enable comprehensive evaluation of tissue function and physiology.
Overall, the characteristics and advantages of a 1.5 Tesla magnetic field make it a versatile, reliable, and cost-effective option for a wide range of clinical applications in Magnetic Resonance Imaging.
The technology behind 1.5 Tesla Magnetic Resonance Imaging (MRI) involves sophisticated equipment and techniques that harness the principles of magnetic resonance to produce detailed images of the body’s internal structures. Here’s an overview of the key components and technologies involved in 1.5T MRI:
Magnet: At the heart of every MRI system is a powerful magnet that generates the main magnetic field. In the case of 1.5T MRI, this magnet produces a magnetic field with a strength of 1.5 Tesla. The magnet is typically a superconducting magnet cooled to extremely low temperatures using liquid helium to maintain its superconducting state.
Gradient Coils: Gradient coils are used to spatially encode the signals from the body, allowing for the creation of detailed cross-sectional images. These coils produce additional magnetic field gradients that vary in strength across the imaging volume.
Radiofrequency (RF) Coils: RF coils are used to transmit radiofrequency pulses into the body and receive the resulting signals emitted by the body’s tissues. These coils come in various designs and configurations, including surface coils placed close to the body part of interest and body coils that surround the entire patient.
Pulse Sequences: Pulse sequences are sets of radiofrequency pulses and magnetic field gradients that are applied during the MRI scan to manipulate the magnetic properties of the tissues and produce images with specific contrasts. Different pulse sequences, such as T1-weighted, T2-weighted, and gradient echo sequences, are used to highlight different tissue characteristics.
Receiver and Signal Processing: The signals received by the RF coils are amplified and processed by sophisticated receiver systems. Signal processing algorithms are then applied to reconstruct the raw data into detailed images of the body’s internal structures.
Software and Reconstruction Algorithms: Advanced software and reconstruction algorithms are used to process the raw MRI data and generate high-quality images. These algorithms correct for various imaging artifacts, such as motion artifacts and magnetic field inhomogeneities, to ensure accurate and reliable imaging results.
Patient Comfort Features: 1.5T MRI systems often include features designed to enhance patient comfort during the scan, such as wide-bore designs to reduce feelings of claustrophobia, noise-reduction technologies, and ergonomic patient positioning systems.
Overall, the technology of 1.5 Tesla Magnetic Resonance Imaging involves a combination of powerful magnets, gradient coils, RF coils, pulse sequences, signal processing, and reconstruction algorithms to produce detailed and clinically valuable images of the body’s internal structures.
The MRI (Magnetic Resonance Imaging) system consists of several basic components that work together to produce detailed images of the body’s internal structures. Here are the key components of an MRI system:
Magnet: The magnet is the core component of the MRI system and generates a strong magnetic field. It is typically a superconducting magnet cooled to extremely low temperatures using liquid helium. The main magnetic field strength in a typical clinical MRI system is 1.5 Tesla (T) or 3 Tesla (T), although higher field strengths are also available in research settings.
Gradient Coils: Gradient coils are additional coils wrapped around the main magnet and used to create small, temporary magnetic field gradients within the imaging volume. These gradients are essential for spatially encoding the MRI signals and producing detailed images.
Radiofrequency (RF) Coils: RF coils are used to transmit radiofrequency pulses into the body and receive the resulting signals emitted by the body’s tissues. RF coils come in various designs, including surface coils placed close to the body part of interest and body coils that surround the entire patient.
Gradient Amplifiers: Gradient amplifiers supply the electrical current needed to energize the gradient coils and create the magnetic field gradients necessary for spatial encoding.
RF Transmit/Receive System: The RF transmit/receive system is responsible for generating the radiofrequency pulses used to excite the hydrogen nuclei in the body and for receiving the resulting MRI signals emitted by the tissues.
Computer System: A powerful computer system controls the operation of the MRI scanner, including the timing and sequencing of RF pulses and gradient pulses, and processes the raw MRI data to generate images. Advanced software and reconstruction algorithms are used for image reconstruction and post-processing.
Patient Table: The patient table is where the patient lies during the MRI scan. It is typically motorized and can move in and out of the MRI scanner to position the patient correctly within the imaging volume.
Operator Console: The operator console is where the MRI technologist or radiologist controls the MRI scanner and monitors the scan in real-time. It contains the user interface, display screens, and controls for adjusting scan parameters.
Safety Systems: MRI systems are equipped with safety systems to ensure the safety of both patients and operators. These systems include monitoring devices to detect motion, temperature sensors to prevent overheating, and emergency shut-off switches.
Overall, these components work together seamlessly to acquire high-quality MRI images for diagnostic purposes, providing valuable information to healthcare providers for the diagnosis and management of various medical conditions.
Clinical applications and utilization of Magnetic Resonance Imaging (MRI) encompass a wide range of medical fields and conditions due to its versatility and ability to produce detailed images of the body’s internal structures. Here are some key clinical applications and utilization of MRI:
Neuroimaging: MRI is extensively used in neurology to visualize the brain, spinal cord, and nerves. It is valuable in diagnosing conditions such as tumors, strokes, multiple sclerosis, traumatic brain injuries, and neurodegenerative disorders like Alzheimer’s disease.
Musculoskeletal Imaging: MRI is highly effective in evaluating musculoskeletal conditions such as ligament and tendon injuries, joint abnormalities, bone fractures, and soft tissue tumors. It provides detailed images of bones, joints, muscles, and cartilage.
Cardiovascular Imaging: MRI plays a crucial role in cardiovascular imaging, including assessment of heart function, detection of heart diseases such as myocardial infarction, cardiomyopathies, and congenital heart defects, as well as evaluation of blood vessels (MR angiography).
Abdominal and Pelvic Imaging: MRI is used to assess abdominal and pelvic organs, including the liver, kidneys, pancreas, gastrointestinal tract, reproductive organs, and pelvic floor. It aids in diagnosing conditions such as liver tumors, pancreatic cancer, and pelvic inflammatory disease.
Oncological Imaging: MRI is valuable in oncology for detecting and staging various cancers, including brain tumors, breast cancer, prostate cancer, and liver metastases. It provides detailed information about tumor size, location, and involvement of adjacent structures.
Breast Imaging: MRI is used as a supplementary imaging modality for breast cancer screening in high-risk individuals and for evaluating breast abnormalities detected on mammography or ultrasound. It can detect small tumors and assess tumor extent.
Functional MRI (fMRI): Functional MRI is used to map brain activity by measuring changes in blood flow and oxygenation. It is employed in research and clinical settings to study brain function, language processing, motor function, and cognitive tasks.
Pediatric Imaging: MRI is widely utilized in pediatric imaging due to its non-invasive nature and lack of ionizing radiation. It is used to evaluate congenital anomalies, neurological conditions, musculoskeletal disorders, and oncological cases in children.
Interventional MRI: MRI-guided interventions, such as MRI-guided biopsies and MRI-guided surgeries, are performed using specialized MRI-compatible instruments and real-time imaging to precisely target and treat lesions.
Overall, MRI is a versatile imaging modality with diverse clinical applications across various medical specialties, providing valuable diagnostic information and guiding treatment decisions for a wide range of conditions.
The role and applications of 1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) in medical fields are extensive due to its ability to produce high-quality images of the body’s internal structures. Here are some key roles and applications of 1.5T MRI across various medical fields:
Neurology: 1.5T MRI is widely used in neurology for imaging the brain, spinal cord, and nerves. It is valuable in diagnosing and monitoring conditions such as brain tumors, stroke, multiple sclerosis, traumatic brain injuries, and neurodegenerative diseases like Alzheimer’s disease and Parkinson’s disease.
Musculoskeletal Imaging: In orthopedics and sports medicine, 1.5T MRI is essential for evaluating musculoskeletal conditions such as ligament and tendon injuries, joint abnormalities, meniscal tears, bone fractures, and soft tissue tumors. It provides detailed images of bones, joints, muscles, and cartilage.
Cardiology: 1.5T MRI plays a crucial role in cardiovascular imaging, including assessment of heart function, detection of heart diseases such as myocardial infarction, cardiomyopathies, and congenital heart defects, as well as evaluation of blood vessels (MR angiography).
Abdominal and Pelvic Imaging: In gastroenterology and urology, 1.5T MRI is used to assess abdominal and pelvic organs, including the liver, kidneys, pancreas, gastrointestinal tract, reproductive organs, and pelvic floor. It aids in diagnosing conditions such as liver tumors, pancreatic cancer, kidney stones, and pelvic inflammatory disease.
Oncology: 1.5T MRI is valuable in oncology for detecting and staging various cancers, including brain tumors, breast cancer, prostate cancer, liver metastases, and musculoskeletal tumors. It provides detailed information about tumor size, location, and involvement of adjacent structures.
Breast Imaging: In breast health, 1.5T MRI is used as a supplementary imaging modality for breast cancer screening in high-risk individuals and for evaluating breast abnormalities detected on mammography or ultrasound. It can detect small tumors and assess tumor extent.
Pediatric Imaging: In pediatrics, 1.5T MRI is widely utilized due to its non-invasive nature and lack of ionizing radiation. It is used to evaluate congenital anomalies, neurological conditions, musculoskeletal disorders, and oncological cases in children.
Functional MRI (fMRI): 1.5T MRI is employed in research and clinical settings for functional MRI (fMRI) studies to map brain activity by measuring changes in blood flow and oxygenation. It is used to study brain function, language processing, motor function, and cognitive tasks.
Overall, 1.5T MRI plays a pivotal role in diagnosing, monitoring, and guiding treatment decisions across various medical fields, providing valuable diagnostic information and contributing to improved patient care and outcomes.
Utilization in Different Body Regions such as Brain, Spine, Joints, etc.
Brain Imaging: 1.5T MRI is extensively utilized for brain imaging to assess various neurological conditions, including brain tumors, strokes, multiple sclerosis, Alzheimer’s disease, and traumatic brain injuries. It provides detailed images of the brain’s anatomy, allowing for accurate diagnosis and treatment planning.
Spine Imaging: In spinal imaging, 1.5T MRI is invaluable for evaluating spinal cord injuries, disc herniations, spinal tumors, degenerative disc diseases, and spinal infections. It offers excellent soft tissue contrast, enabling visualization of spinal cord compression, nerve root impingement, and structural abnormalities.
Musculoskeletal Imaging: 1.5T MRI plays a crucial role in musculoskeletal imaging by providing detailed evaluation of joints, muscles, ligaments, tendons, and bones. It is commonly used to diagnose sports injuries, osteoarthritis, rheumatoid arthritis, ligament tears (such as ACL and PCL tears), meniscal tears, and cartilage abnormalities.
Abdominal Imaging: In abdominal imaging, 1.5T MRI is employed to assess abdominal organs such as the liver, pancreas, kidneys, spleen, and gastrointestinal tract. It aids in diagnosing liver lesions, pancreatic tumors, renal cysts, bowel obstructions, and inflammatory bowel diseases (such as Crohn’s disease and ulcerative colitis).
Pelvic Imaging: 1.5T MRI is utilized for pelvic imaging to evaluate pelvic organs, including the uterus, ovaries, prostate, bladder, and pelvic floor muscles. It is valuable in diagnosing conditions such as uterine fibroids, ovarian cysts, prostate cancer, bladder tumors, and pelvic organ prolapse.
Breast Imaging: In breast imaging, 1.5T MRI is used as a supplemental tool for breast cancer screening and evaluation of breast abnormalities. It provides detailed images of breast tissue, facilitating the detection of small tumors, evaluation of tumor extent, and assessment of breast implant integrity.
Cardiovascular Imaging: 1.5T MRI is employed in cardiovascular imaging to assess heart function, myocardial viability, and vascular anatomy. It aids in diagnosing conditions such as myocardial infarction, cardiomyopathies, congenital heart defects, and aortic aneurysms.
Peripheral Vascular Imaging: 1.5T MRI is used for peripheral vascular imaging to evaluate blood vessels in the extremities. It is valuable for diagnosing peripheral arterial disease, deep vein thrombosis, vascular malformations, and peripheral artery aneurysms.
Overall, 1.5T MRI is utilized in various body regions for diagnosing a wide range of medical conditions, providing clinicians with detailed anatomical information for accurate diagnosis and treatment planning.
High resolution and contrast are two essential characteristics of Magnetic Resonance Imaging (MRI) that contribute to its effectiveness in diagnostic imaging. Here’s an overview of these key features:
High Resolution: MRI offers high spatial resolution, allowing for detailed visualization of anatomical structures within the body. This high resolution is achieved through various factors:
Magnet Strength: MRI scanners with higher magnetic field strengths, such as 1.5 Tesla (1.5T) or 3 Tesla (3T), generally provide better spatial resolution compared to lower field strengths.
Gradient Coils: Gradient coils within the MRI scanner create spatial variations in the magnetic field, enabling precise localization of signals from different regions of the body. Higher gradient strengths contribute to improved spatial resolution.
Receiver Coils: Specialized radiofrequency (RF) receiver coils placed near the area of interest enhance signal reception, leading to improved spatial resolution in the resulting images.
Pulse Sequences: Different pulse sequences, such as T1-weighted, T2-weighted, and gradient echo sequences, offer varying levels of spatial resolution. Adjusting parameters within these sequences can further optimize resolution based on the imaging requirements.
High Contrast: MRI produces images with excellent tissue contrast, allowing for differentiation between different types of tissues based on their inherent magnetic properties. Several factors contribute to achieving high contrast:
Tissue Relaxation Times: MRI exploits the differences in tissue relaxation times (T1 and T2) to generate contrast between tissues. Tissues with shorter T1 or T2 relaxation times appear brighter or darker, respectively, in the resulting images.
Contrast Agents: Contrast agents, such as gadolinium-based agents, can be administered intravenously to enhance the contrast between tissues, particularly in vascular or perfusion studies.
Pulse Sequences: Different pulse sequences manipulate tissue relaxation times to optimize contrast between tissues of interest. For example, T1-weighted sequences provide excellent contrast between fat and water, while T2-weighted sequences enhance contrast between fluid-filled structures and surrounding tissues.
Imaging Parameters: Adjusting imaging parameters such as repetition time (TR), echo time (TE), and inversion time (TI) can further optimize contrast based on the specific imaging goals and tissue characteristics.
High resolution and contrast in MRI images enable radiologists and clinicians to accurately visualize anatomical structures, detect abnormalities, and make informed diagnostic and treatment decisions across various medical specialties.
Fast scan times and reduced waiting periods are crucial advantages of Magnetic Resonance Imaging (MRI) that contribute to its efficiency and patient comfort. Here’s how these features are achieved:
Advanced Hardware and Software: Modern MRI systems are equipped with advanced hardware components and software algorithms designed to optimize scan times. This includes powerful gradient coils, high-performance RF coils, and sophisticated pulse sequences that enable rapid image acquisition.
Gradient Coils: Gradient coils play a key role in accelerating scan times by rapidly switching magnetic field gradients during image acquisition. These gradients encode spatial information and allow for faster data sampling, reducing the time needed to acquire images.
Parallel Imaging Techniques: Parallel imaging techniques, such as Sensitivity Encoding (SENSE) and Generalized Autocalibrating Partially Parallel Acquisitions (GRAPPA), enable faster image acquisition by simultaneously acquiring multiple image data sets with fewer phase-encoding steps. This reduces the overall scan time while maintaining image quality.
Fast Imaging Sequences: MRI sequences optimized for speed, such as fast spin-echo (FSE) and echo-planar imaging (EPI), enable rapid acquisition of images in a single breath-hold or short scan time. These sequences are particularly useful for dynamic studies and imaging of moving organs, such as the heart and abdomen.
Motion Correction Techniques: Motion artifacts can prolong scan times and degrade image quality. Advanced motion correction techniques, such as prospective motion correction and navigator-based techniques, help mitigate motion artifacts and improve scan efficiency by reducing the need for repeat scans.
Patient Comfort Features: MRI systems with wide-bore designs and patient-friendly features enhance patient comfort and compliance during scans. These designs accommodate larger patients and reduce feelings of claustrophobia, resulting in smoother and more efficient scanning sessions.
Optimized Protocols: Radiologists and technologists optimize MRI protocols based on the specific imaging requirements and clinical indications, tailoring scan parameters to achieve the desired diagnostic information while minimizing scan times.
Efficient Workflow Practices: Efficient workflow practices, such as streamlined patient preparation, optimized scheduling, and prioritization of urgent cases, help minimize waiting periods and maximize MRI scanner utilization.
Overall, fast scan times and reduced waiting periods in MRI imaging contribute to improved patient throughput, enhanced patient experience, and efficient utilization of imaging resources in clinical settings.
Information obtained with 1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) encompasses detailed anatomical and functional data across various body regions, providing valuable diagnostic insights for a wide range of medical conditions. Here are some key types of information obtained with 1.5T MRI:
Anatomical Imaging: 1.5T MRI produces high-resolution images that delineate the anatomy of organs, tissues, and structures within the body. It provides detailed visualization of soft tissues, bones, organs, blood vessels, and nerves, allowing for the detection of abnormalities, lesions, and structural variations.
Tissue Characterization: MRI offers excellent tissue contrast, enabling the differentiation of various types of tissues based on their inherent magnetic properties and relaxation times. This facilitates the characterization of tissues, identification of abnormalities, and assessment of tissue composition, such as distinguishing between healthy and pathological tissues.
Functional Imaging: Functional MRI (fMRI) studies performed at 1.5T capture dynamic changes in tissue function and metabolism. fMRI techniques, such as blood oxygen level-dependent (BOLD) imaging, allow for mapping of brain activity, localization of functional areas within the brain, and assessment of neurological functions such as language processing, motor function, and cognitive tasks.
Vascular Imaging: 1.5T MRI is utilized for vascular imaging, including magnetic resonance angiography (MRA), to assess blood vessels and vascular anatomy. It provides detailed visualization of arteries and veins, aiding in the diagnosis of vascular abnormalities, stenosis, aneurysms, and vascular malformations.
Diffusion-weighted Imaging (DWI): DWI performed at 1.5T MRI assesses the diffusion of water molecules within tissues, providing information about tissue cellularity, microstructure, and integrity. DWI is valuable for detecting acute stroke, evaluating tumor aggressiveness, and assessing tissue viability in ischemic conditions.
Dynamic Contrast-enhanced Imaging: Dynamic contrast-enhanced MRI (DCE-MRI) performed at 1.5T monitors the uptake and washout of contrast agents in tissues over time, providing information about tissue perfusion, vascularity, and angiogenesis. DCE-MRI is used in oncology for assessing tumor vascularity and response to therapy.
Functional Connectomics: Advanced MRI techniques, such as resting-state functional connectivity MRI (rs-fMRI), performed at 1.5T, analyze spontaneous low-frequency fluctuations in brain activity to map functional connectivity networks within the brain. This aids in understanding brain connectivity patterns and neural network organization in health and disease.
Spectroscopy: Magnetic resonance spectroscopy (MRS) performed at 1.5T provides metabolic information by measuring the concentrations of specific metabolites within tissues. MRS is used to assess brain metabolism, characterize brain lesions, and monitor treatment response in neurological disorders.
Overall, 1.5T MRI offers a comprehensive range of information, including detailed anatomical imaging, functional data, tissue characterization, and vascular assessment, facilitating accurate diagnosis, treatment planning, and monitoring of various medical conditions across multiple body systems.
The ability of 1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) to provide functional information is a key advantage that enhances its diagnostic capabilities in various medical applications. Here’s how 1.5T MRI facilitates the assessment of functional information:
Functional MRI (fMRI): 1.5T MRI is widely used for functional MRI studies, which assess brain activity by detecting changes in blood flow and oxygenation levels associated with neural activity. fMRI enables the mapping of functional areas of the brain involved in specific tasks or cognitive processes, such as motor function, language processing, memory, and sensory perception. By measuring brain activation patterns, fMRI helps neuroscientists and clinicians understand brain function, localize cortical areas responsible for specific functions, and diagnose neurological conditions affecting brain activity.
Diffusion Tensor Imaging (DTI): DTI is a specialized MRI technique performed at 1.5T that evaluates the microstructural integrity and organization of white matter tracts in the brain. By measuring the direction and magnitude of water diffusion within brain tissue, DTI provides information about the structural connectivity of neural pathways. DTI is valuable for assessing conditions involving white matter abnormalities, such as traumatic brain injury, stroke, multiple sclerosis, and neurodegenerative diseases.
Resting-State Functional Connectivity MRI (rs-fMRI): Rs-fMRI is an MRI technique performed at 1.5T that evaluates functional connectivity patterns in the brain during rest. By analyzing spontaneous low-frequency fluctuations in blood oxygen level-dependent (BOLD) signals, rs-fMRI identifies networks of brain regions that exhibit synchronized activity, known as resting-state networks (RSNs). Rs-fMRI helps researchers and clinicians understand the functional organization of the brain, characterize alterations in brain connectivity associated with neurological disorders, and assess the impact of interventions on brain network connectivity.
Perfusion Imaging: Dynamic contrast-enhanced MRI (DCE-MRI) and arterial spin labeling (ASL) are perfusion imaging techniques performed at 1.5T MRI that assess cerebral blood flow and tissue perfusion in the brain. Perfusion imaging provides functional information about regional blood flow patterns, vascular supply to brain tissue, and tissue perfusion deficits associated with cerebrovascular diseases, brain tumors, and neurodegenerative disorders. It aids in diagnosing and monitoring conditions affecting cerebral perfusion, such as ischemic stroke, brain tumors, and vascular dementia.
Spectroscopy: Magnetic resonance spectroscopy (MRS) is an MRI technique performed at 1.5T that measures the concentrations of specific metabolites within tissues, providing insights into tissue metabolism and biochemical composition. MRS is used to assess brain metabolism, detect metabolic abnormalities associated with neurological disorders, and monitor treatment response in conditions such as brain tumors, epilepsy, and neurodegenerative diseases. By evaluating metabolic markers, MRS enhances the functional characterization of brain lesions and aids in treatment planning.
Overall, 1.5T MRI enables the assessment of functional information through advanced imaging techniques such as fMRI, DTI, rs-fMRI, perfusion imaging, and spectroscopy, enhancing the understanding of brain function, connectivity, and metabolism in health and disease. These functional MRI modalities play a crucial role in neuroscience research, clinical neuroimaging, and personalized medicine, providing valuable insights into brain function and dysfunction.
1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) is considered safe for patients when appropriate safety guidelines and protocols are followed. Here are key aspects related to the safety of 1.5T MRI:
Magnetic Field Safety: The main safety concern with MRI is the strong magnetic field generated by the MRI scanner. A 1.5T MRI scanner produces a powerful magnetic field that can attract ferromagnetic objects and exert forces on magnetic materials. To ensure safety, all individuals entering the MRI room must be screened for ferromagnetic objects, such as pacemakers, implants, jewelry, and medical devices, which can pose risks if brought into the magnetic field.
Implant and Device Safety: Patients with certain medical implants, devices, or foreign bodies may require special considerations before undergoing an MRI scan at 1.5T. Implants containing ferromagnetic materials, electronic devices, or components that can be affected by the magnetic field, such as cardiac pacemakers, defibrillators, neurostimulators, cochlear implants, and certain vascular stents, may pose risks or require specific scanning protocols. Patients should inform the MRI technologist and radiologist about any implants, devices, or foreign bodies they have before the scan.
Contrast Agent Safety: Gadolinium-based contrast agents (GBCAs) are sometimes used during MRI scans to enhance image contrast for certain studies. While generally considered safe, GBCAs may rarely cause adverse reactions, including allergic reactions and nephrogenic systemic fibrosis (NSF) in patients with impaired kidney function. Radiologists carefully evaluate the necessity of contrast administration based on patient history, clinical indications, and potential risks.
Radiofrequency (RF) Safety: MRI involves the use of RF energy to manipulate the magnetic resonance signals emitted by the body’s tissues. RF energy deposition in the body is carefully controlled to prevent excessive heating of tissues, particularly in patients with metallic implants or conductive materials. MRI technologists monitor RF power deposition levels and adjust scanning parameters to ensure patient safety and minimize RF-related heating effects.
Acoustic Noise Safety: MRI scanners produce loud acoustic noise during scanning, which can be discomforting for patients and may require the use of ear protection. Patients are provided with earplugs or headphones to mitigate the noise level and protect their hearing during the MRI scan.
Pregnancy Safety: While there is no evidence to suggest that MRI at 1.5T poses specific risks to pregnant women or their unborn babies, caution is typically exercised, particularly during the first trimester of pregnancy. MRI scans during pregnancy are generally avoided unless medically necessary and performed under the guidance of a healthcare provider, considering the potential benefits versus risks.
Overall, 1.5T MRI is considered safe for most patients when appropriate safety measures are implemented, and patient-specific factors are considered to ensure safe scanning conditions and optimal imaging quality. Healthcare providers, including MRI technologists and radiologists, play a crucial role in assessing patient safety and minimizing potential risks associated with MRI scanning.
Several precautions are taken to ensure patient safety during Magnetic Resonance Imaging (MRI) scanning, especially at 1.5 Tesla (1.5T) field strength. Here are key precautions:
Screening for Ferromagnetic Objects: Before entering the MRI scanner room, all patients and personnel are screened for ferromagnetic objects, including metallic implants, devices, jewelry, and other items that can be attracted to the strong magnetic field. Patients are instructed to remove all metal objects and inform the MRI staff about any implants or devices they may have.
Patient Screening Questionnaire: Patients are typically asked to complete a screening questionnaire to identify any contraindications or conditions that may affect their safety during the MRI scan. This includes questions about previous surgeries, medical implants, medical history, allergies, and pregnancy status.
Implant and Device Compatibility: Patients with medical implants, devices, or foreign bodies that may be affected by the magnetic field, such as cardiac pacemakers, neurostimulators, cochlear implants, and certain vascular stents, undergo thorough evaluation for compatibility with MRI. In some cases, specific scanning protocols or alternative imaging modalities may be recommended.
Patient Monitoring: Patients undergoing MRI are closely monitored throughout the scanning procedure by trained MRI technologists and medical personnel. Continuous communication with the patient is maintained to ensure comfort and address any concerns or issues that may arise during the scan.
MRI Safety Zones: Controlled access zones are established around the MRI scanner to restrict entry and prevent unauthorized personnel from entering the magnetic field area. Clear signage and safety protocols are in place to ensure compliance with safety guidelines and prevent accidents.
Patient Positioning and Immobilization: Patients are positioned carefully on the MRI table and secured with immobilization devices, such as foam pads or straps, to minimize movement during the scan. Immobilization helps maintain image quality and reduces the risk of motion artifacts.
Emergency Preparedness: MRI facilities are equipped with emergency response plans and safety protocols to address potential emergencies, such as magnet quenching, patient distress, or medical emergencies during scanning. Trained personnel are available to respond promptly to any safety-related incidents.
Patient Education and Reassurance: Before the MRI scan, patients receive detailed instructions about the procedure, safety precautions, and what to expect during the scan. Education and reassurance help alleviate anxiety and promote cooperation and compliance with safety instructions.
Pregnancy Screening and Safety: Female patients of childbearing age are screened for pregnancy before undergoing MRI, especially if contrast agents are planned for use. MRI scans during pregnancy are generally avoided unless medically necessary and performed under the guidance of a healthcare provider, considering the potential risks versus benefits.
By implementing these precautions and safety measures, healthcare providers ensure the safe and effective performance of MRI scans, minimize risks to patients, and maintain high standards of patient care and safety.
Advancements in imaging techniques have revolutionized the field of medical diagnostics, allowing for more precise, efficient, and non-invasive evaluation of various anatomical and physiological processes. Some notable advancements include:
High-Resolution Imaging: Advances in MRI and CT technology have led to the development of scanners capable of producing higher resolution images with enhanced spatial and contrast resolution. This allows for better visualization of anatomical structures and subtle pathological changes, leading to improved diagnostic accuracy.
Functional Imaging: Functional imaging techniques such as functional MRI (fMRI), positron emission tomography (PET), and single-photon emission computed tomography (SPECT) provide insights into brain function, metabolism, and blood flow. These techniques are valuable for mapping brain activity, diagnosing neurological disorders, and monitoring treatment response.
Multimodal Imaging: Integration of multiple imaging modalities, such as PET/CT and PET/MRI, allows for complementary information to be obtained in a single imaging session. Multimodal imaging enhances diagnostic accuracy, improves localization of abnormalities, and provides comprehensive information for treatment planning.
Dynamic Imaging: Dynamic imaging techniques, including dynamic contrast-enhanced MRI (DCE-MRI) and dynamic contrast-enhanced CT (DCE-CT), enable real-time visualization of physiological processes such as blood flow, tissue perfusion, and contrast agent kinetics. Dynamic imaging is particularly useful for assessing tumor vascularity, monitoring treatment response, and evaluating perfusion deficits in ischemic conditions.
Diffusion-Weighted Imaging (DWI): DWI is an MRI technique that measures the random motion of water molecules within tissues. DWI provides information about tissue microstructure, cellularity, and integrity, and is valuable for diagnosing acute stroke, evaluating tumor aggressiveness, and assessing white matter abnormalities in neurological disorders.
Molecular Imaging: Molecular imaging techniques, including PET imaging with radiotracers and contrast-enhanced molecular MRI, allow for the visualization of molecular processes at the cellular and molecular level. Molecular imaging is used for cancer staging, detecting molecular targets, and monitoring disease progression and treatment response.
Artificial Intelligence (AI) in Imaging: AI and machine learning algorithms are increasingly being used to analyze medical images, improve image quality, and assist radiologists in interpretation. AI-based tools can automate image segmentation, detect abnormalities, and predict patient outcomes, leading to faster and more accurate diagnosis.
Advanced Image Reconstruction Techniques: Iterative reconstruction algorithms in CT imaging and parallel imaging techniques in MRI enable faster image acquisition, reduced radiation dose, and improved image quality. These advanced reconstruction techniques enhance diagnostic capabilities while minimizing patient exposure to radiation.
Quantitative Imaging Biomarkers: Quantitative imaging biomarkers derived from imaging data, such as tumor volume, diffusion metrics, and perfusion parameters, provide objective measures of disease severity, treatment response, and prognosis. Quantitative imaging biomarkers aid in personalized medicine, treatment planning, and clinical decision-making.
Overall, advancements in imaging techniques have transformed medical imaging, enabling earlier detection, more accurate diagnosis, and targeted therapy for a wide range of medical conditions. Continued research and innovation in imaging technology hold promise for further improvements in patient care and outcomes.
The future of 1.5 Tesla Magnetic Resonance Imaging (1.5T MRI) is poised to see several exciting developments that will further enhance its capabilities and impact on healthcare. Here are some anticipated advancements:
Improved Image Quality: Ongoing research and development efforts aim to further enhance the image quality of 1.5T MRI scans. This includes advancements in coil design, pulse sequence optimization, and image reconstruction techniques to achieve higher spatial resolution, improved tissue contrast, and reduced artifacts.
Functional and Molecular Imaging: Future innovations in 1.5T MRI technology will likely expand its capabilities for functional and molecular imaging. This includes the development of advanced techniques such as diffusion tensor imaging (DTI), magnetic resonance spectroscopy (MRS), and molecular imaging with targeted contrast agents, enabling non-invasive assessment of tissue microstructure, metabolism, and molecular markers of disease.
Quantitative Imaging Biomarkers: 1.5T MRI is expected to play a key role in the development and validation of quantitative imaging biomarkers for various disease processes. These biomarkers, derived from quantitative analysis of MRI data, can provide objective measures of disease severity, treatment response, and prognosis, facilitating personalized medicine and precision healthcare.
Artificial Intelligence (AI) Integration: Integration of AI and machine learning algorithms into 1.5T MRI systems will enhance workflow efficiency, automate image analysis tasks, and improve diagnostic accuracy. AI-based applications for image reconstruction, segmentation, and computer-aided diagnosis will streamline interpretation and decision-making, leading to more efficient and precise patient care.
Functional Connectomics: With advancements in functional MRI (fMRI) techniques, 1.5T MRI will continue to contribute to the field of connectomics by mapping functional brain networks and understanding brain connectivity patterns in health and disease. Future developments may enable comprehensive functional connectomic analysis using 1.5T MRI, shedding light on neural circuitry and brain-behavior relationships.
Point-of-Care and Portable MRI: Miniaturization of MRI technology and development of portable or point-of-care 1.5T MRI systems may enable wider accessibility to MRI imaging in diverse clinical settings, including remote and resource-limited areas. Portable MRI devices could revolutionize healthcare delivery by bringing advanced imaging capabilities closer to patients, improving diagnosis, and facilitating early intervention.
Personalized Imaging Protocols: Advancements in personalized medicine and patient-specific imaging protocols will enable tailored MRI examinations based on individual patient characteristics, clinical indications, and treatment objectives. Adaptive imaging techniques and real-time feedback mechanisms will optimize imaging parameters and protocols to maximize diagnostic yield while minimizing scan time and patient discomfort.
Integration with Multimodal Imaging: Integration of 1.5T MRI with other imaging modalities, such as PET, CT, and ultrasound, will enable comprehensive multi-parametric imaging for more accurate diagnosis and treatment planning. Hybrid imaging platforms and integrated imaging suites will facilitate seamless data fusion and correlation across different imaging modalities, offering a holistic approach to patient evaluation.
Overall, the future of 1.5T MRI is characterized by continued innovation, expanding clinical applications, and integration with emerging technologies, paving the way for more personalized, precise, and impactful diagnostic imaging in healthcare.
The evolution and changing role of Magnetic Resonance Imaging (MRI), particularly at 1.5 Tesla (1.5T), in clinical applications reflect ongoing advancements in technology, expanding indications, and innovative approaches to patient care. Here are some key aspects of its evolution and changing role:
Expanded Clinical Indications: Over the years, 1.5T MRI has expanded its role beyond traditional anatomical imaging to include functional, metabolic, and molecular imaging. It is now used across various medical specialties, including neurology, oncology, cardiology, orthopedics, and gastroenterology, for a wide range of diagnostic purposes.
Improved Image Quality and Resolution: Advances in hardware and software have led to significant improvements in image quality and spatial resolution in 1.5T MRI. High-resolution imaging techniques allow for better visualization of anatomical structures and pathological changes, enabling more accurate diagnosis and treatment planning.
Functional and Physiological Imaging: Functional MRI (fMRI), diffusion-weighted imaging (DWI), perfusion imaging, and spectroscopy are among the functional and physiological imaging techniques increasingly utilized in clinical practice. These techniques provide valuable information about tissue function, microstructure, and metabolism, aiding in the diagnosis and management of neurological, oncological, and cardiovascular conditions.
Quantitative Imaging Biomarkers: 1.5T MRI is increasingly used for quantitative imaging, where objective measurements of tissue properties, such as diffusion, perfusion, and relaxation times, serve as imaging biomarkers for disease characterization, treatment response assessment, and prognostication.
Precision Medicine and Personalized Imaging: With the advent of precision medicine, 1.5T MRI is playing a vital role in tailoring imaging protocols and treatment strategies to individual patient characteristics and disease phenotypes. Personalized imaging approaches optimize scan parameters, sequences, and contrast administration based on specific patient needs, optimizing diagnostic accuracy and therapeutic outcomes.
Integration with Multimodal Imaging: Integration of 1.5T MRI with other imaging modalities, such as positron emission tomography (PET), computed tomography (CT), and ultrasound, enhances diagnostic capabilities and provides complementary information for comprehensive patient evaluation. Multimodal imaging approaches enable better tissue characterization, lesion detection, and treatment planning across various medical disciplines.
Advancements in Interventional MRI: In addition to diagnostic imaging, 1.5T MRI is increasingly used for interventional procedures, such as MRI-guided biopsies, ablations, and surgeries. Real-time imaging and navigation capabilities allow for precise targeting of lesions and minimally invasive interventions, reducing procedural risks and improving patient outcomes.
Research and Innovation: Ongoing research and innovation in MRI technology continue to drive advancements in 1.5T MRI, leading to novel imaging techniques, sequence optimization, and software developments. Collaborations between researchers, clinicians, and industry partners foster innovation and translate research findings into clinical practice, further expanding the role of 1.5T MRI in healthcare.
Overall, the evolution and changing role of 1.5T MRI in clinical applications reflect its versatility, utility, and ongoing contributions to modern healthcare, with continued advancements poised to further enhance its diagnostic and therapeutic capabilities in the future.
Future directions and potential improvements in Magnetic Resonance Imaging (MRI), particularly at 1.5 Tesla (1.5T), are driven by ongoing technological advancements, emerging research trends, and evolving healthcare needs. Here are some potential directions and improvements:
Enhanced Image Quality and Spatial Resolution: Continued advancements in hardware and software technology aim to further improve image quality and spatial resolution in 1.5T MRI. This includes the development of higher-performance gradient systems, advanced coil designs, and optimized imaging sequences to achieve sharper, clearer images with enhanced tissue contrast and anatomical detail.
Functional and Molecular Imaging: Future innovations in 1.5T MRI technology will likely focus on expanding its capabilities for functional and molecular imaging. This includes the development of new imaging biomarkers and techniques for assessing tissue function, metabolism, and molecular signatures of disease. Advances in spectroscopic imaging, diffusion imaging, and contrast-enhanced techniques will enable more comprehensive characterization of tissue pathology and physiological processes.
Quantitative Imaging Biomarkers: The future of 1.5T MRI involves the refinement and validation of quantitative imaging biomarkers for various disease processes. Quantitative MRI techniques, such as diffusion tensor imaging (DTI), perfusion imaging, and magnetic resonance elastography (MRE), will be further optimized to provide objective measures of tissue microstructure, perfusion, and mechanical properties. These biomarkers will play an increasingly important role in disease diagnosis, treatment monitoring, and personalized medicine.
Artificial Intelligence (AI) Integration: Integration of AI and machine learning algorithms into 1.5T MRI systems will enhance image analysis, workflow efficiency, and diagnostic accuracy. AI-based applications for image reconstruction, segmentation, and computer-aided diagnosis will automate routine tasks, assist radiologists in interpretation, and enable quantitative analysis of imaging data. AI-driven predictive models may also help in predicting disease outcomes and treatment response based on MRI findings.
Multimodal Imaging Integration: Integration of 1.5T MRI with other imaging modalities, such as positron emission tomography (PET), computed tomography (CT), and ultrasound, will enable comprehensive multi-parametric imaging for improved diagnosis and treatment planning. Hybrid imaging platforms and integrated imaging suites will facilitate seamless data fusion and correlation across different imaging modalities, providing a more holistic approach to patient evaluation.
Point-of-Care and Portable MRI: Miniaturization of MRI technology and the development of portable or point-of-care 1.5T MRI systems may enable wider accessibility to MRI imaging in diverse clinical settings, including remote and resource-limited areas. Portable MRI devices could revolutionize healthcare delivery by bringing advanced imaging capabilities closer to patients, improving diagnosis, and facilitating early intervention.
Theranostic Applications: 1.5T MRI has the potential to serve as a theranostic tool by combining diagnostic imaging with targeted therapies. MRI-guided interventions, such as focused ultrasound ablation and drug delivery, allow for precise targeting of lesions while minimizing damage to surrounding tissues. Future developments in theranostic agents and MRI-compatible treatment modalities will enable personalized and targeted therapies based on MRI findings.
Overall, the future of 1.5T MRI involves continuous innovation, integration with emerging technologies, and the translation of research findings into clinical practice to improve patient care and outcomes. Continued collaboration between researchers, clinicians, and industry partners will drive advancements in MRI technology and shape its future directions in healthcare.
Patient rights and important considerations regarding Magnetic Resonance Imaging (MRI) scanning are essential aspects of healthcare delivery to ensure patient safety, comfort, and well-being. Here are some key rights and considerations for patients undergoing MRI scanning:
Informed Consent: Patients have the right to receive comprehensive information about the MRI procedure, including its purpose, benefits, potential risks, and alternatives. Informed consent should be obtained before the scan, and patients should have the opportunity to ask questions and address any concerns.
Safety Precautions: Patient safety is paramount during MRI scanning. Patients must disclose any relevant medical history, including allergies, prior surgeries, implanted devices (e.g., pacemakers, cochlear implants), or other conditions that may affect the MRI procedure. MRI technologists and healthcare providers should adhere to strict safety protocols to minimize risks associated with magnetic fields and radiofrequency energy.
Comfort and Support: Patients should be provided with appropriate accommodations to ensure comfort during the MRI scan. This may include the provision of earplugs or headphones to reduce noise, the use of cushions or positioning aids to maintain comfort during the scan, and the availability of a call button or intercom for communication with MRI staff.
Privacy and Dignity: Patients have the right to privacy and dignity during the MRI scanning process. Facilities should ensure adequate privacy measures, such as private changing rooms and screening areas, to protect patient confidentiality. Modesty garments or drapes may be provided to maintain patient dignity during the scan.
Accommodations for Special Needs: Patients with special needs, such as claustrophobia, mobility limitations, or sensory sensitivities, should receive appropriate accommodations to ensure a safe and comfortable MRI experience. This may include the use of open MRI systems, sedation or anesthesia for anxious patients, or the presence of a caregiver or support person during the scan.
Radiation Safety: While MRI does not use ionizing radiation, patients should be informed about the potential risks associated with contrast agents used in some MRI scans. Patients with a history of allergies, kidney disease, or other medical conditions should be screened for contraindications to contrast administration, and appropriate safety measures should be implemented.
Inclusion and Cultural Sensitivity: Healthcare providers should ensure cultural sensitivity and inclusivity when interacting with patients undergoing MRI scanning. Patients from diverse cultural backgrounds may have unique beliefs, preferences, or concerns related to medical procedures, and efforts should be made to accommodate their individual needs and preferences.
Communication and Education: Patients have the right to receive clear and understandable information about the MRI procedure, including pre-scan instructions, expected duration of the scan, and post-scan care. Effective communication and patient education help alleviate anxiety, promote cooperation during the scan, and empower patients to participate in their care.
Feedback and Resolution of Concerns: Patients should be encouraged to provide feedback about their MRI experience, including any concerns or issues encountered during the scan. Healthcare facilities should have mechanisms in place to address patient feedback, resolve concerns promptly, and ensure continuous quality improvement in MRI services.
Follow-Up Care: Patients undergoing MRI scanning should receive appropriate follow-up care based on the findings of the scan and any recommendations from healthcare providers. This may include additional diagnostic tests, referrals to specialists, or discussions about treatment options, as necessary.
By upholding these patient rights and considerations, healthcare providers can ensure a positive and patient-centered MRI experience, promote patient safety and well-being, and uphold the highest standards of care in MRI imaging.
Privacy and data protection are crucial considerations in Magnetic Resonance Imaging (MRI) to safeguard patient confidentiality, comply with regulatory requirements, and ensure the secure handling of sensitive medical information. Here are key aspects of privacy and data protection in MRI:
Confidentiality: Patient confidentiality is paramount in MRI imaging. Healthcare providers must ensure that patient information, including personal and medical data, is kept confidential and only accessed by authorized personnel involved in the patient’s care.
Data Encryption: MRI systems and associated software should employ encryption techniques to secure patient data during transmission and storage. This helps prevent unauthorized access to sensitive information and ensures data integrity.
Access Controls: Access to MRI systems and patient data should be restricted to authorized personnel with appropriate credentials and access permissions. Role-based access controls should be implemented to limit access to patient information based on job responsibilities.
Audit Trails: MRI systems should maintain audit trails that record user activities, including access to patient data and system operations. Audit trails enable accountability and traceability of data access, facilitating investigations in case of security incidents or breaches.
Compliance with Regulations: Healthcare providers and MRI facilities must comply with relevant privacy and data protection regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or the General Data Protection Regulation (GDPR) in the European Union. Compliance entails implementing policies, procedures, and technical safeguards to protect patient privacy and ensure lawful processing of personal data.
Data Minimization: MRI facilities should practice data minimization by collecting and retaining only the minimum amount of patient information necessary for diagnostic purposes. Unnecessary data should be promptly deleted or anonymized to reduce the risk of unauthorized access or misuse.
Patient Consent: Patients should provide informed consent for the collection, processing, and sharing of their medical information for MRI purposes. Consent forms should clearly explain the nature of the MRI procedure, the use of patient data, and any potential risks or implications.
Secure Data Storage: Patient data obtained through MRI scans should be stored securely in electronic health record (EHR) systems or other designated repositories with robust security measures, such as encryption, access controls, and regular data backups. Physical safeguards, such as locked storage cabinets or rooms, should also be in place to protect patient records.
Data Retention Policies: MRI facilities should establish data retention policies specifying the length of time patient data will be retained and the criteria for data deletion or archiving. Retention periods should align with legal requirements and clinical needs, and data disposal should be conducted securely to prevent unauthorized access.
Employee Training: Healthcare personnel involved in MRI imaging should receive regular training on privacy and data protection practices, including handling patient information, maintaining confidentiality, and reporting security incidents. Training programs help raise awareness and promote a culture of privacy and compliance within the organization.
By adhering to these privacy and data protection measures, MRI facilities can uphold patient privacy rights, mitigate security risks, and maintain the trust and confidence of patients in the handling of their sensitive medical information.
Patient rights and preferences during the scanning process in Magnetic Resonance Imaging (MRI) are essential considerations to ensure a positive and comfortable experience for individuals undergoing MRI examinations. Here are key rights and preferences that should be respected:
Informed Consent: Patients have the right to provide informed consent before undergoing an MRI scan. This includes receiving detailed information about the procedure, potential risks, benefits, alternatives, and any necessary preparations. Patients should also have the opportunity to ask questions and express their concerns before consenting to the scan.
Privacy and Dignity: Patients have the right to privacy and dignity during the scanning process. Facilities should provide appropriate changing areas and ensure that patients are adequately covered during the procedure to maintain their dignity. Modesty garments or drapes may be offered to enhance patient comfort and privacy.
Comfortable Environment: Patients should be provided with a comfortable environment during the MRI scan. This includes ensuring appropriate room temperature, lighting, and noise levels to promote relaxation and reduce anxiety. Facilities may offer amenities such as earplugs, headphones, or music to enhance patient comfort during the scan.
Communication and Education: Patients have the right to receive clear and understandable information about the MRI scan, including what to expect during the procedure, how long it will last, and any sensations they may experience. Healthcare providers should communicate with patients in a compassionate and reassuring manner, addressing any concerns or questions they may have.
Empowerment and Control: Patients should be empowered to participate in decisions about their care during the scanning process. This includes having the ability to communicate their preferences, such as requesting breaks during the scan or informing technologists about any discomfort or anxiety they may be experiencing. Facilities should strive to accommodate patient preferences whenever possible to enhance their sense of control.
Safety Measures: Patients have the right to receive information about safety measures taken during the MRI scan to ensure their well-being. This includes explanations about the magnetic field, radiofrequency energy, and any potential risks associated with the procedure. Patients should also be informed about safety protocols, such as removing metal objects and jewelry, to prevent accidents during the scan.
Support Persons: Patients may have the preference to have a support person accompany them during the MRI scan for emotional support and reassurance. Facilities should accommodate this preference whenever possible, ensuring that support persons are briefed on safety guidelines and remain in designated areas during the procedure.
Feedback and Follow-Up: Patients should be encouraged to provide feedback about their MRI experience, including any suggestions for improvement or concerns they may have encountered. Facilities should have mechanisms in place to collect patient feedback and address any issues raised. Additionally, patients should receive appropriate follow-up care based on the results of the MRI scan and any recommendations from healthcare providers.
By respecting these rights and preferences, MRI facilities can create a patient-centered environment that prioritizes the comfort, well-being, and empowerment of individuals undergoing MRI examinations. This approach fosters trust, improves patient satisfaction, and enhances the overall quality of care provided during the scanning process.
Frequently Asked Questions

Get a Free Second Opinion
Experienced Burtom Medical Team is Ready to Help

I consent to Burtom Health Group using my aforesaid personal data for the purposes described in this notice and understand that I can withdraw my consent at any time by sending a request to info@burtom.com.