Burtom ‣ Technologies ‣ Positron Emission Tomography Computed Tomography (PET CT)
Language: 🇬🇧 English | 🇹🇷 Türkçe
Positron Emission Tomography Computed Tomography (PET CT) Overview

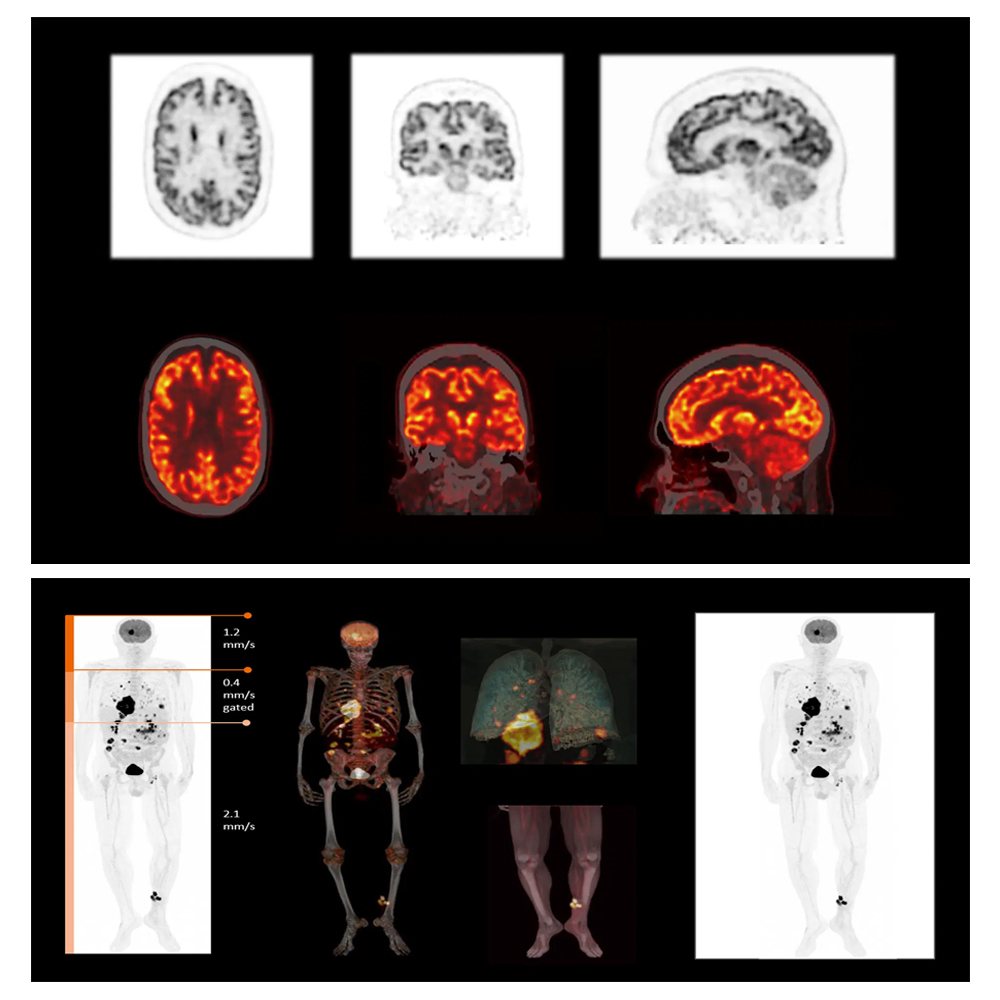
 Positron Emission Tomography Computed Tomography (PET-CT) is a sophisticated imaging modality that merges two powerful imaging techniques, Positron Emission Tomography (PET) and Computed Tomography (CT), into a single procedure. PET imaging detects gamma rays emitted by a radioactive tracer that is injected into the body, highlighting areas with high metabolic activity, such as cancerous tumors. Meanwhile, CT utilizes X-rays to create detailed cross-sectional images of the body’s internal structures, providing anatomical information. By combining PET and CT technologies, PET-CT scans offer a comprehensive evaluation of both functional and structural aspects of tissues and organs, enabling healthcare professionals to accurately diagnose and stage various medical conditions, including cancer, neurological disorders, and cardiovascular diseases. This integrated approach enhances diagnostic accuracy, improves treatment planning, and facilitates better patient management by providing a more complete understanding of the underlying pathophysiology. Additionally, PET-CT scans play a crucial role in monitoring treatment response and disease progression, guiding therapeutic decisions, and optimizing patient outcomes. Overall, PET-CT imaging represents a valuable tool in modern medicine, allowing for precise localization, characterization, and monitoring of diseases, ultimately leading to improved patient care.
Positron Emission Tomography Computed Tomography (PET-CT) is a sophisticated imaging modality that merges two powerful imaging techniques, Positron Emission Tomography (PET) and Computed Tomography (CT), into a single procedure. PET imaging detects gamma rays emitted by a radioactive tracer that is injected into the body, highlighting areas with high metabolic activity, such as cancerous tumors. Meanwhile, CT utilizes X-rays to create detailed cross-sectional images of the body’s internal structures, providing anatomical information. By combining PET and CT technologies, PET-CT scans offer a comprehensive evaluation of both functional and structural aspects of tissues and organs, enabling healthcare professionals to accurately diagnose and stage various medical conditions, including cancer, neurological disorders, and cardiovascular diseases. This integrated approach enhances diagnostic accuracy, improves treatment planning, and facilitates better patient management by providing a more complete understanding of the underlying pathophysiology. Additionally, PET-CT scans play a crucial role in monitoring treatment response and disease progression, guiding therapeutic decisions, and optimizing patient outcomes. Overall, PET-CT imaging represents a valuable tool in modern medicine, allowing for precise localization, characterization, and monitoring of diseases, ultimately leading to improved patient care. What is Positron Emission Tomography (PET) and How Does it Work?

Positron Emission Tomography (PET) is a medical imaging technique that visualizes metabolic processes in the body. It works by detecting gamma rays emitted by a radioactive tracer, known as a radiopharmaceutical, which is introduced into the body. These tracers are designed to accumulate in specific tissues or organs based on their metabolic activity. As the tracer undergoes radioactive decay, it emits positrons (positively charged electrons), which travel a short distance before encountering electrons in surrounding tissues. Upon collision, positrons annihilate with electrons, producing pairs of gamma rays that travel in opposite directions. PET scanners detect these gamma rays using detectors positioned around the body, allowing the reconstruction of three-dimensional images that reflect the distribution and intensity of metabolic activity within tissues or organs. This metabolic information is valuable for diagnosing and staging various medical conditions, including cancer, neurological disorders, and cardiovascular diseases, and for assessing treatment response.
Basic Principles and Principles of PET
The basic principles of Positron Emission Tomography (PET) revolve around the detection of gamma rays emitted by positron-emitting radiotracers, which are introduced into the body and accumulate in tissues or organs based on their metabolic activity. The principles of PET imaging involve the detection of these gamma rays using detectors positioned around the body, allowing for the reconstruction of three-dimensional images that reflect the distribution and intensity of metabolic activity within tissues or organs. This metabolic information is crucial for diagnosing and staging various medical conditions, including cancer, neurological disorders, and cardiovascular diseases, and for assessing treatment response.
Patient Experience During PET-CT Scanning
During PET-CT scanning, patients typically experience a non-invasive procedure that involves lying comfortably on a table that moves into the scanner. The PET-CT scanner resembles a large, tunnel-like machine. Patients may need to fast for a few hours before the scan, depending on the specific instructions provided by their healthcare provider. Once positioned on the table, patients are required to remain still during the scanning process to ensure clear and accurate images.
For the PET component of the scan, patients receive a small amount of radioactive tracer, usually through an intravenous injection. This tracer travels to the targeted area in the body and emits positrons, which are detected by the PET scanner to produce metabolic images.
During the CT component of the scan, which typically follows the PET scan, patients may receive contrast dye through an intravenous line to enhance the visibility of certain tissues and organs. The CT scanner uses X-rays to create detailed cross-sectional images of the body’s internal structures.
Throughout the PET-CT scanning process, patients are monitored by trained technologists or healthcare professionals who ensure their comfort and safety. The entire procedure usually takes about 30 to 60 minutes to complete.
While some patients may experience mild discomfort from the intravenous injection or lying still for an extended period, PET-CT scanning is generally well-tolerated by most individuals. It’s essential for patients to communicate any concerns or discomfort they may experience during the procedure to the healthcare team, who can address their needs promptly.
Combined Positron Emission Tomography and Computed Tomography (PET-CT)
Combined Positron Emission Tomography and Computed Tomography (PET-CT) is an advanced medical imaging technique that integrates two powerful imaging modalities, Positron Emission Tomography (PET) and Computed Tomography (CT), into a single examination. This combined approach provides both functional and anatomical information about the body in a single imaging session, allowing for more accurate and comprehensive assessment of various medical conditions.
In a PET-CT scan, a patient is positioned on a table that moves through the PET and CT scanners. During the PET component of the scan, a radiotracer is injected into the patient’s body, which emits positrons that interact with nearby electrons, resulting in the emission of gamma rays. These gamma rays are detected by the PET scanner and used to create images that show the metabolic activity of tissues and organs.
Simultaneously, the CT component of the scan utilizes X-rays to create detailed cross-sectional images of the body’s internal structures, providing anatomical information about bones, organs, and tissues. By combining the functional information from PET with the anatomical information from CT, PET-CT scans offer a more comprehensive evaluation of the body, allowing healthcare professionals to better diagnose and stage various medical conditions, such as cancer, neurological disorders, and cardiovascular diseases.
PET-CT scans are widely used in clinical practice for cancer staging and treatment planning, as well as for diagnosing and monitoring other conditions. The integration of PET and CT technologies in a single imaging session improves diagnostic accuracy, enhances treatment planning, and facilitates better patient management by providing a more complete understanding of the underlying disease processes.
PET-CT System and Basic Components
The PET-CT system consists of several key components that work together to perform the combined Positron Emission Tomography and Computed Tomography (PET-CT) imaging. These components include:
- PET Scanner: The PET scanner is designed to detect and measure the gamma rays emitted by the radioactive tracer injected into the patient’s body. It consists of multiple detector rings that surround the patient, allowing for the detection of gamma rays from multiple angles. The PET scanner produces functional images that show the distribution of the radiotracer in the body, highlighting areas of metabolic activity.
- CT Scanner: The CT scanner uses X-rays to create detailed cross-sectional images of the body’s internal structures, including bones, organs, and tissues. It consists of an X-ray tube that rotates around the patient and a detector array that measures the X-rays passing through the body. The CT scanner produces anatomical images that provide information about the structure and location of tissues and organs.
- Patient Table: The patient table is a movable platform on which the patient lies during the PET-CT scan. It is designed to move smoothly and precisely through the PET and CT scanners, allowing for accurate alignment of the images acquired by both modalities.
- Computer System: The computer system is the central component of the PET-CT system, responsible for controlling the operation of the scanners, acquiring and processing image data, and generating the final fused PET-CT images. Advanced software algorithms are used to combine the functional PET images with the anatomical CT images, providing comprehensive diagnostic information.
- Injection System: The injection system is used to administer the radioactive tracer into the patient’s bloodstream before the PET-CT scan. It consists of a syringe containing the radiotracer and a programmable injector that delivers the tracer at a controlled rate.
- Display and Control Console: The display and control console allows the technologist or radiologist to monitor the PET-CT scan in real-time, adjust imaging parameters, and review acquired images. It typically includes a computer monitor, keyboard, and mouse for user interaction.
Overall, these components work together seamlessly to acquire and process PET and CT images simultaneously, providing valuable functional and anatomical information for diagnostic purposes in various medical applications.
The combined use of Positron Emission Tomography (PET) and Computed Tomography (CT) in PET-CT imaging offers several advantages over standalone PET or CT imaging. Some of the key advantages include:
- Improved Diagnostic Accuracy: PET-CT imaging provides both functional and anatomical information in a single examination, allowing for more accurate localization and characterization of abnormalities. By combining metabolic data from PET with anatomical details from CT, PET-CT scans enhance diagnostic accuracy and facilitate better disease detection and characterization.
- Precise Anatomic Localization: PET-CT allows for precise localization of metabolic abnormalities within the anatomical context provided by CT. This helps in accurately identifying the source and extent of abnormalities, such as tumors, inflammatory lesions, or areas of infection, leading to more targeted and effective treatment planning.
- Enhanced Staging and Treatment Planning: PET-CT is particularly valuable for cancer staging and treatment planning. It provides comprehensive information about the metabolic activity of tumors and their surrounding tissues, as well as detailed anatomical images of adjacent structures and organs. This integrated information aids in staging cancer accurately, assessing treatment response, and planning optimal treatment strategies, including surgery, radiation therapy, or chemotherapy.
- Reduction of False Positives and Negatives: PET-CT imaging reduces the occurrence of false positives and false negatives compared to standalone PET or CT imaging. By correlating metabolic abnormalities with their precise anatomical locations, PET-CT helps in differentiating between benign and malignant lesions, minimizing the likelihood of misdiagnosis and unnecessary interventions.
- Single Examination, Reduced Radiation Exposure: PET-CT combines PET and CT scans into a single examination, eliminating the need for separate imaging sessions. This not only saves time and resources but also reduces overall radiation exposure for patients compared to undergoing standalone PET and CT scans separately.
- Improved Patient Management: The comprehensive information provided by PET-CT scans facilitates better patient management by enabling more informed clinical decision-making. Healthcare providers can use PET-CT findings to tailor personalized treatment plans, monitor disease progression, and assess treatment response more accurately, ultimately leading to improved patient outcomes.
Overall, the combined use of PET and CT in PET-CT imaging offers significant advantages in terms of diagnostic accuracy, precise anatomical localization, cancer staging, treatment planning, radiation dose reduction, and improved patient management.
PET-CT scanning is performed in a specialized imaging facility equipped with both a PET scanner and a CT scanner. The procedure typically involves the following steps:
- Preparation: Before the PET-CT scan, patients may be instructed to fast for a few hours to ensure optimal imaging results, particularly for certain types of scans. Patients are also advised to inform their healthcare provider about any medications they are taking, as some medications may interfere with the imaging process.
- Injection of Radiotracer: Once the patient is ready, a radiotracer is injected into the patient’s bloodstream. The choice of radiotracer depends on the specific imaging purpose, such as evaluating cancer, neurological disorders, or cardiovascular diseases. The radiotracer is designed to accumulate in specific tissues or organs based on their metabolic activity.
- Waiting Period: After the radiotracer injection, patients may need to wait for a certain period, known as the uptake time, to allow the tracer to distribute throughout the body and accumulate in the target tissues or organs. The uptake time varies depending on the specific radiotracer used and the imaging protocol.
- PET Imaging: Once the uptake time has elapsed, the patient is positioned on the PET scanner table. The PET scanner detects gamma rays emitted by the radiotracer as it undergoes radioactive decay within the body. These gamma rays are produced when positrons emitted by the radiotracer collide with electrons in the body tissues. The PET scanner rotates around the patient, acquiring a series of PET images from different angles.
- CT Imaging: After the PET scan, the patient may undergo a CT scan immediately or shortly afterward, depending on the specific imaging protocol. The CT scan uses X-rays to create detailed cross-sectional images of the body’s internal structures, providing anatomical information about bones, organs, and tissues.
- Fusion of PET and CT Images: The PET and CT images acquired during the scan are then fused together using specialized software to create integrated PET-CT images. This fusion process combines the functional information from PET with the anatomical information from CT, allowing for more comprehensive and accurate evaluation of the target tissues or organs.
- Image Interpretation: The fused PET-CT images are interpreted by a trained radiologist or nuclear medicine physician, who analyzes the images to assess metabolic activity, detect abnormalities, and make diagnostic evaluations. The findings are then reported to the referring healthcare provider for further management.
Overall, PET-CT scanning is a non-invasive imaging procedure that combines PET and CT technologies to provide comprehensive diagnostic information about various medical conditions.
The preparation process before undergoing a PET-CT scan typically involves the following steps:
- Consultation with Healthcare Provider: Patients may have a consultation with their healthcare provider, usually a radiologist or nuclear medicine physician, to discuss the purpose of the PET-CT scan, review their medical history, and address any concerns or questions they may have about the procedure.
- Medication Review: Patients should inform their healthcare provider about any medications they are currently taking, including prescription medications, over-the-counter drugs, and supplements. Some medications may need to be adjusted or temporarily discontinued before the scan, depending on their potential to interfere with the imaging process.
- Fasting: In some cases, patients may be instructed to fast for a certain period before the PET-CT scan, typically for several hours. Fasting helps improve imaging quality by reducing background metabolic activity in the body, particularly for scans focusing on specific organs or conditions.
- Hydration: Patients are usually encouraged to stay well-hydrated before the PET-CT scan by drinking plenty of water. Adequate hydration helps improve the distribution of the radiotracer within the body and enhances imaging quality.
- Blood Glucose Levels: For certain types of PET-CT scans, such as those aimed at evaluating cancer or neurological disorders, patients may be required to maintain stable blood glucose levels before the scan. High blood sugar levels can interfere with the uptake of the radiotracer by cells and affect imaging results.
- Pregnancy and Breastfeeding: Female patients should inform their healthcare provider if they are pregnant or breastfeeding, as some radiotracers used in PET-CT scans may pose risks to the developing fetus or nursing infant. In such cases, alternative imaging modalities or precautions may be considered.
- Clothing and Personal Items: Patients are typically advised to wear comfortable, loose-fitting clothing without metal objects or jewelry for the scan. Metal objects can interfere with the imaging process and may need to be removed before the procedure. Patients may also be asked to remove items such as watches, belts, and hairpins.
- Arrival Time: Patients should arrive at the imaging facility at the scheduled time and may be asked to complete any necessary paperwork or consent forms before the scan. It’s essential to arrive on time to ensure that the scan can be performed according to the planned schedule.
Overall, following the preparation instructions provided by the healthcare provider helps ensure the success and accuracy of the PET-CT scan, leading to optimal diagnostic outcomes.
Ensuring patient comfort during a PET-CT scan is a priority for healthcare providers. Several measures are taken to maximize patient comfort throughout the scanning process:
- Explanation and Education: Before the scan, healthcare providers explain the procedure in detail, addressing any concerns or questions the patient may have. Educating the patient about what to expect during the scan helps alleviate anxiety and promotes a sense of control.
- Comfortable Environment: The scanning room is designed to provide a comfortable environment for the patient. The room is typically temperature-controlled, and patients are provided with blankets or pillows if needed to enhance comfort during the scan.
- Positioning and Support: Patients are positioned comfortably on the PET-CT scanner table, and supportive padding may be used to ensure proper alignment and minimize discomfort during the scan. Patients are encouraged to communicate any discomfort or pain to the healthcare team, who can make adjustments as needed.
- Communication: Open communication between the patient and healthcare team is essential throughout the scanning process. Patients are encouraged to notify the technologist or radiologist if they experience any discomfort or anxiety during the scan. Healthcare providers reassure patients and address their concerns promptly to ensure their comfort and well-being.
- Relaxation Techniques: Patients are encouraged to practice relaxation techniques, such as deep breathing or visualization, to help reduce anxiety and promote relaxation during the scan. Some imaging facilities may offer additional amenities, such as music or ambient lighting, to create a calming atmosphere.
- Minimizing Scan Duration: PET-CT scans are typically performed as quickly as possible to minimize the duration of the procedure and reduce patient discomfort. Advanced imaging techniques and protocols are used to acquire images efficiently while maintaining high image quality.
- Patient Monitoring: Throughout the scan, patients are monitored by trained technologists or healthcare professionals to ensure their comfort and safety. Patients are provided with a call button or intercom system to communicate with the healthcare team if needed during the scan.
Overall, healthcare providers strive to create a supportive and comfortable environment for patients undergoing PET-CT scans, addressing their individual needs and concerns to ensure a positive experience.
In neurology, PET-CT scanning plays a vital role in the diagnosis and monitoring of various neurological disorders by providing valuable insights into brain metabolism, blood flow, and neuronal function. Some of the key neurological disorders diagnosed and monitored using PET-CT imaging include:
- Alzheimer’s Disease (AD): PET-CT scans are used to detect characteristic patterns of amyloid-beta and tau protein deposition in the brain, which are hallmarks of Alzheimer’s disease. PET-CT imaging helps in the early diagnosis and staging of AD, monitoring disease progression, and evaluating response to treatment.
- Parkinson’s Disease (PD): PET-CT scans are utilized to assess dopamine metabolism and neuronal activity in the brain regions affected by Parkinson’s disease. PET-CT imaging aids in the differential diagnosis of PD from other movement disorders, monitoring disease progression, and evaluating the efficacy of dopaminergic medications and surgical interventions.
- Epilepsy: PET-CT scans are employed in the evaluation of patients with epilepsy to localize epileptogenic foci and identify regions of abnormal brain metabolism or perfusion. PET-CT imaging helps in surgical planning for patients with drug-resistant epilepsy by identifying the precise location of seizure onset and guiding the resection of epileptic lesions.
- Brain Tumors: PET-CT scans are used to characterize brain tumors based on their metabolic activity, providing valuable information for tumor grading, staging, and treatment planning. PET-CT imaging aids in differentiating between benign and malignant brain tumors, assessing tumor response to therapy, and detecting tumor recurrence.
- Cerebrovascular Diseases: PET-CT scans are employed in the evaluation of patients with cerebrovascular diseases, such as ischemic stroke, hemorrhagic stroke, and cerebral ischemia. PET-CT imaging helps in assessing cerebral blood flow, metabolism, and tissue viability, guiding treatment decisions and predicting patient outcomes.
- Neurodegenerative Disorders: PET-CT scans are used in the evaluation of various neurodegenerative disorders, including Huntington’s disease, frontotemporal dementia, and Lewy body dementia. PET-CT imaging provides valuable information about neuronal loss, neurotransmitter function, and brain metabolism, aiding in the differential diagnosis and management of these conditions.
- Traumatic Brain Injury (TBI): PET-CT scans are utilized in the assessment of patients with traumatic brain injury to evaluate the extent of brain damage, assess cerebral perfusion and metabolism, and predict patient outcomes. PET-CT imaging helps in guiding treatment decisions and monitoring recovery in patients with TBI.
Overall, PET-CT scanning plays a crucial role in the diagnosis and monitoring of various neurological disorders by providing valuable insights into brain function, metabolism, and perfusion. It helps neurologists make informed clinical decisions, tailor treatment plans, and monitor disease progression in their patients.
PET-CT imaging offers several advantages and benefits compared to standalone PET or CT imaging. Some of the key advantages include:
- Comprehensive Evaluation: PET-CT provides both functional and anatomical information in a single examination, allowing for a more comprehensive evaluation of the body. This integrated approach enhances diagnostic accuracy by correlating metabolic data from PET with detailed anatomical images from CT.
- Improved Diagnostic Accuracy: PET-CT scans offer higher diagnostic accuracy compared to standalone PET or CT imaging, particularly in oncology. The combination of metabolic information from PET with anatomical details from CT helps in better characterizing abnormalities, distinguishing between benign and malignant lesions, and accurately localizing disease sites.
- Enhanced Cancer Staging: PET-CT is highly valuable for cancer staging as it helps in detecting primary tumors, assessing the extent of disease spread (metastasis), and identifying involvement of nearby lymph nodes or distant organs. Accurate cancer staging is crucial for determining prognosis and guiding treatment decisions.
- Optimized Treatment Planning: PET-CT aids in optimizing treatment planning for cancer patients by providing valuable information about tumor metabolism, size, and location. It helps oncologists determine the most appropriate treatment approach, including surgery, radiation therapy, chemotherapy, or targeted therapy, based on the specific characteristics of the tumor.
- Monitoring Treatment Response: PET-CT is used to monitor the response to cancer treatment by assessing changes in tumor metabolism and size over time. It helps healthcare providers evaluate the effectiveness of chemotherapy, radiation therapy, immunotherapy, or other targeted therapies and make adjustments to the treatment plan as needed.
- Reduced False Positives and Negatives: PET-CT imaging reduces the occurrence of false positives and false negatives compared to standalone PET or CT imaging. By combining metabolic data from PET with anatomical information from CT, PET-CT scans improve the accuracy of lesion detection and characterization, minimizing the likelihood of misdiagnosis and unnecessary interventions.
- Single Examination, Reduced Radiation Exposure: PET-CT combines PET and CT scans into a single examination, eliminating the need for separate imaging sessions. This not only saves time and resources but also reduces overall radiation exposure for patients compared to undergoing standalone PET and CT scans separately.
- Guidance for Interventional Procedures: PET-CT scans can guide interventional procedures, such as biopsy or needle aspiration, by precisely localizing abnormal areas identified on imaging. This targeted approach improves the accuracy of tissue sampling and reduces the risk of sampling errors.
Overall, PET-CT imaging offers numerous advantages and benefits, including improved diagnostic accuracy, optimized treatment planning, enhanced cancer staging, and reduced radiation exposure, making it a valuable tool in modern medicine for the evaluation and management of various medical conditions.
One of the significant advantages of PET-CT imaging is its ability to combine metabolic and anatomical information in a single examination. This integrated approach offers several benefits in clinical practice:
- Comprehensive Evaluation: PET-CT provides a comprehensive evaluation of the body by combining functional information from PET, which depicts metabolic activity, with detailed anatomical images from CT. This integration allows for a more thorough assessment of various medical conditions, including cancer, neurological disorders, and cardiovascular diseases.
- Improved Lesion Characterization: By correlating metabolic data from PET with anatomical details from CT, PET-CT imaging enhances the characterization of lesions. It helps differentiate between benign and malignant lesions, identify areas of abnormal metabolic activity, and precisely localize disease sites within the body.
- Accurate Cancer Staging: PET-CT is highly valuable for cancer staging as it combines information about tumor metabolism (PET) with anatomical details of tumor size, location, and involvement of nearby structures (CT). This integrated approach improves the accuracy of cancer staging, guiding treatment decisions and predicting patient prognosis.
- Optimized Treatment Planning: PET-CT aids in optimizing treatment planning for cancer patients by providing comprehensive information about tumor characteristics and extent of disease spread. It helps oncologists determine the most appropriate treatment approach, including surgery, radiation therapy, chemotherapy, or targeted therapy, based on both metabolic and anatomical considerations.
- Monitoring Treatment Response: PET-CT is used to monitor the response to cancer treatment by assessing changes in tumor metabolism and size over time. This integrated approach allows healthcare providers to evaluate the effectiveness of chemotherapy, radiation therapy, immunotherapy, or other targeted therapies and make adjustments to the treatment plan as needed.
- Reduction of False Positives and Negatives: PET-CT imaging reduces the occurrence of false positives and false negatives compared to standalone PET or CT imaging. By combining metabolic and anatomical information, PET-CT scans improve the accuracy of lesion detection and characterization, minimizing the likelihood of misdiagnosis and unnecessary interventions.
Overall, the ability of PET-CT imaging to combine metabolic and anatomical information in a single examination offers significant advantages in clinical practice, including enhanced lesion characterization, accurate cancer staging, optimized treatment planning, and improved monitoring of treatment response. This integrated approach contributes to better patient care and management across various medical specialties.
PET-CT imaging involves the use of ionizing radiation, which raises concerns about radiation exposure. However, measures are in place to ensure patient safety and minimize radiation risks during PET-CT scanning:
- Radiotracer Selection: Radiotracers used in PET imaging have short half-lives, meaning they decay quickly and lose their radioactivity within a short period. This minimizes the duration of radiation exposure to the patient.
- Radiotracer Dose Optimization: Radiotracer doses are carefully optimized to achieve the desired imaging results while minimizing radiation exposure to the patient. Radiotracer doses are personalized based on factors such as patient weight, body composition, and specific imaging needs.
- ALARA Principle: Healthcare providers follow the ALARA (As Low As Reasonably Achievable) principle to minimize radiation exposure during PET-CT scanning. This principle emphasizes the importance of using the lowest possible radiation dose that still provides diagnostically acceptable images.
- Technological Advances: Advanced PET-CT systems incorporate technological innovations, such as time-of-flight (TOF) imaging and iterative reconstruction algorithms, which improve image quality and allow for reduced radiation doses without compromising diagnostic accuracy.
- Shielding and Collimation: Lead shielding and collimation techniques are used to limit radiation exposure to surrounding tissues and organs not under examination. This helps to focus the radiation beam on the target area of interest while minimizing exposure to healthy tissues.
- Patient Positioning: Proper patient positioning is essential to ensure that the radiation beam is directed only to the areas being imaged, minimizing exposure to adjacent tissues and organs.
- Pregnancy and Radiation Safety: Pregnant patients are carefully evaluated for the potential risks and benefits of PET-CT scanning. Whenever possible, PET-CT imaging is deferred during pregnancy to avoid potential harm to the fetus. If imaging is deemed necessary, precautions are taken to minimize radiation exposure to the fetus.
- Radiation Monitoring and Regulation: Healthcare facilities adhere to strict radiation safety guidelines and regulations established by regulatory agencies, such as the Nuclear Regulatory Commission (NRC) in the United States. Radiation exposure levels are monitored and recorded, and personnel are trained in radiation safety protocols.
Overall, PET-CT imaging is performed with careful consideration of radiation safety measures to ensure patient well-being and minimize radiation risks. By following established protocols and utilizing advanced technologies, healthcare providers strive to maintain a balance between achieving diagnostic accuracy and ensuring patient safety during PET-CT scanning.
Ensuring patient safety during PET-CT scanning involves implementing various measures to minimize risks and address potential concerns. Some key measures include:
- Patient Screening: Before the scan, patients undergo thorough screening to assess their medical history, including any allergies, previous reactions to contrast agents, or underlying health conditions that may impact the procedure. This helps identify potential contraindications and ensures patient suitability for the scan.
- Radiation Safety: PET-CT scanners are equipped with safety features to limit radiation exposure to patients. These include automatic exposure control mechanisms, dose optimization protocols, and shielding to protect surrounding tissues from unnecessary radiation exposure.
- Radiation Dose Monitoring: Radiation doses delivered during PET-CT scanning are closely monitored and recorded to ensure that they adhere to established safety guidelines and regulatory standards. Healthcare providers track cumulative radiation exposure over time and take appropriate measures to minimize unnecessary exposure.
- Patient Education: Patients receive comprehensive education about the PET-CT procedure, including its purpose, benefits, potential risks, and any preparatory steps they need to take. Clear instructions are provided regarding fasting requirements, medication adjustments, and other pre-scan preparations to ensure optimal imaging quality and safety.
- Informed Consent: Patients are fully informed about the risks and benefits of PET-CT scanning and are asked to provide informed consent before the procedure. This involves discussing potential risks, such as allergic reactions to contrast agents or radiation exposure, and addressing any concerns or questions the patient may have.
- Allergy and Anaphylaxis Management: Patients with a history of allergic reactions to contrast agents are carefully evaluated, and appropriate measures are taken to minimize the risk of an allergic reaction during the scan. Precautionary measures, such as pre-medication with antihistamines or corticosteroids, may be administered to reduce the likelihood of an adverse reaction.
- Patient Monitoring: Patients undergoing PET-CT scanning are closely monitored throughout the procedure to ensure their safety and well-being. Vital signs, including heart rate, blood pressure, and oxygen saturation, may be monitored continuously to detect any signs of distress or adverse reactions promptly.
- Emergency Preparedness: Healthcare providers are trained in emergency procedures and equipped to handle potential complications that may arise during PET-CT scanning, such as allergic reactions, contrast extravasation, or medical emergencies. Emergency medications, resuscitation equipment, and access to advanced life support are readily available to address any unforeseen circumstances.
By implementing these measures, healthcare providers strive to ensure the safety and well-being of patients undergoing PET-CT scanning, while also optimizing the quality and diagnostic accuracy of the imaging procedure.
The evaluation of PET-CT scan results involves a systematic analysis of both metabolic and anatomical information obtained from the imaging study. Key aspects of the evaluation process include:
- Image Interpretation: Radiologists, nuclear medicine physicians, or other qualified specialists interpret PET-CT images to identify areas of abnormal metabolic activity and correlate them with corresponding anatomical structures. They analyze the distribution, intensity, and patterns of tracer uptake in various regions of the body to detect and characterize abnormalities.
- Lesion Detection and Localization: PET-CT scans are assessed for the presence of abnormal metabolic activity suggestive of pathological lesions, such as tumors, inflammatory lesions, or areas of infection. Lesions are localized within specific anatomical regions using the corresponding CT images, facilitating accurate lesion detection and localization.
- Semi-Quantitative Analysis: Quantitative measures, such as standardized uptake values (SUVs), are calculated to quantify the intensity of tracer uptake within identified lesions. SUVs provide objective measures of metabolic activity and can help differentiate between benign and malignant lesions, assess treatment response, and monitor disease progression over time.
- Comparative Analysis: PET-CT scan results may be compared with previous imaging studies, such as PET scans, CT scans, or other modalities, to assess changes in metabolic activity or lesion characteristics over time. Comparative analysis aids in evaluating treatment response, detecting disease progression or recurrence, and guiding further management decisions.
- Diagnostic Interpretation: The findings of PET-CT scan results are interpreted in the context of the patient’s clinical history, symptoms, laboratory tests, and other relevant imaging studies. Diagnostic interpretations consider the likelihood of various differential diagnoses and aim to provide clinically relevant information to guide patient management.
- Multidisciplinary Review: In complex cases or situations requiring specialized expertise, PET-CT scan results may be reviewed by a multidisciplinary team of healthcare professionals, including radiologists, nuclear medicine physicians, oncologists, surgeons, and other specialists. Collaborative review facilitates comprehensive evaluation and ensures optimal patient care.
- Communication of Findings: The findings of PET-CT scan results are communicated to referring physicians and other members of the healthcare team responsible for the patient’s care. Clear and concise reporting of findings, including relevant clinical implications and recommendations, facilitates informed decision-making and appropriate patient management.
Overall, the evaluation of PET-CT scan results involves a comprehensive analysis of metabolic and anatomical information to accurately detect, characterize, and interpret abnormalities, guiding clinical management and treatment decisions for patients across various medical specialties.
PET-CT results play a crucial role in treatment planning for various medical conditions, particularly in oncology. The information obtained from PET-CT scans guides healthcare providers in developing personalized treatment strategies tailored to each patient’s specific disease characteristics. Here are some key ways in which PET-CT results are used in treatment planning:
- Tumor Localization and Staging: PET-CT imaging helps localize primary tumors and assess the extent of disease spread (staging) by identifying metastatic lesions and evaluating lymph node involvement. Accurate tumor localization and staging are essential for determining the appropriate treatment approach, such as surgery, radiation therapy, or systemic therapy.
- Treatment Selection: PET-CT results provide valuable information about tumor characteristics, including metabolic activity, size, and distribution. This information guides healthcare providers in selecting the most appropriate treatment modalities, such as surgery, chemotherapy, immunotherapy, targeted therapy, or a combination of treatments, based on the specific features of the tumor and its response to therapy.
- Assessment of Treatment Response: PET-CT scans are used to monitor the response to cancer treatment by evaluating changes in tumor metabolism and size over time. Response assessment helps healthcare providers determine the effectiveness of chemotherapy, radiation therapy, immunotherapy, or other targeted therapies and make adjustments to the treatment plan as needed.
- Delineation of Target Volumes: PET-CT imaging aids in delineating target volumes for radiation therapy planning by accurately identifying areas of tumor involvement and metabolic activity. This helps radiation oncologists optimize treatment delivery, spare healthy tissues, and minimize radiation-related side effects while effectively targeting tumor cells.
- Evaluation of Residual Disease: PET-CT scans are used to assess residual disease after initial treatment, such as surgery or chemotherapy, to determine the need for additional therapy or to guide further treatment decisions. Detection of residual disease helps healthcare providers tailor ongoing management strategies to achieve optimal disease control and patient outcomes.
- Prediction of Prognosis: PET-CT results provide prognostic information by assessing tumor characteristics, such as metabolic activity and tumor burden. This information helps healthcare providers predict patient outcomes, including disease recurrence, progression-free survival, and overall survival, and tailor treatment plans accordingly.
- Clinical Trial Eligibility: PET-CT results may influence eligibility criteria for participation in clinical trials evaluating novel treatment approaches or investigational therapies. Patients with specific tumor characteristics identified on PET-CT scans may be eligible for targeted therapies or experimental treatments being studied in clinical trials.
Overall, PET-CT results play a pivotal role in treatment planning by providing valuable information about tumor characteristics, treatment response, and prognosis, enabling personalized and effective management strategies for patients with various medical conditions, particularly cancer.
Technological developments and innovations in PET-CT have significantly advanced the field of medical imaging, enhancing diagnostic capabilities, improving patient outcomes, and facilitating personalized treatment approaches. Some notable advancements include:
- Improved Image Quality: Technological advancements in PET-CT scanners have led to improved image quality, resolution, and sensitivity. High-definition detectors, time-of-flight (TOF) imaging, and advanced reconstruction algorithms enhance spatial resolution and signal-to-noise ratio, allowing for better visualization of small lesions and subtle metabolic abnormalities.
- Quantitative Imaging: Innovations in PET-CT technology enable quantitative analysis of metabolic activity using standardized uptake values (SUVs) and other quantitative metrics. Quantitative imaging provides objective measures of tracer uptake, facilitating accurate lesion characterization, treatment response assessment, and prognostic evaluation.
- Integrated Molecular Imaging: PET-CT scanners are increasingly equipped with additional imaging modalities, such as magnetic resonance imaging (MRI) or single-photon emission computed tomography (SPECT), allowing for integrated molecular imaging. Multimodal imaging combines complementary functional and anatomical information, offering a comprehensive evaluation of disease processes and improving diagnostic accuracy.
- Dynamic Imaging Techniques: Advanced PET-CT scanners support dynamic imaging techniques, such as dynamic PET and dynamic contrast-enhanced CT, which capture temporal changes in tracer uptake and tissue perfusion. Dynamic imaging provides insights into physiological processes, pharmacokinetics, and treatment response dynamics, enhancing the understanding of disease mechanisms and guiding therapeutic interventions.
- Radiomics and Machine Learning: Radiomics and machine learning techniques are increasingly utilized in PET-CT imaging for quantitative analysis of imaging features and extraction of predictive biomarkers. These computational approaches enable the extraction of quantitative imaging biomarkers from PET-CT data, facilitating precision medicine approaches, patient stratification, and outcome prediction in various medical conditions.
- Total-Body PET-CT: Total-body PET-CT scanners have been developed to perform whole-body imaging in a single examination, allowing for comprehensive assessment of disease burden and distribution throughout the body. Total-body PET-CT offers advantages in oncology, particularly for staging, treatment planning, and monitoring of systemic diseases.
- Radiation Dose Reduction: Ongoing efforts focus on reducing radiation exposure associated with PET-CT imaging while maintaining diagnostic accuracy. Innovations in dose optimization algorithms, iterative reconstruction techniques, and low-dose protocols aim to minimize radiation dose without compromising image quality, improving patient safety and reducing potential long-term risks.
Overall, technological developments and innovations in PET-CT imaging continue to drive advancements in medical imaging, enabling more precise diagnosis, personalized treatment planning, and improved patient outcomes across various medical specialties.
Patient rights and important considerations regarding PET-CT scanning encompass various aspects aimed at ensuring patient safety, comfort, and informed decision-making throughout the imaging process. Some key rights and considerations include:
- Informed Consent: Patients have the right to receive comprehensive information about the PET-CT procedure, including its purpose, benefits, potential risks, and alternative options. Informed consent ensures that patients understand the nature of the imaging procedure and can make autonomous decisions about their healthcare.
- Privacy and Confidentiality: Patients’ privacy and confidentiality must be respected throughout the PET-CT imaging process. Healthcare providers should adhere to strict confidentiality policies and protect patients’ personal health information in accordance with applicable privacy laws and regulations.
- Safety Measures: Patients have the right to receive safe and high-quality care during PET-CT scanning. Healthcare facilities should adhere to established safety protocols and guidelines to minimize radiation exposure, prevent allergic reactions to contrast agents, and ensure the overall safety of the imaging procedure.
- Patient Education: Patients have the right to receive education and guidance about preparatory steps, such as fasting requirements, medication adjustments, and other pre-scan instructions, to ensure optimal imaging quality and safety. Patient education empowers patients to actively participate in their healthcare and contribute to the success of the imaging procedure.
- Comfort and Support: Patients should be provided with a comfortable and supportive environment during PET-CT scanning to alleviate anxiety and discomfort. Healthcare providers should address patients’ concerns, provide reassurance, and offer appropriate accommodations, such as blankets, pillows, and music, to enhance their overall experience.
- Respect for Dignity and Autonomy: Patients have the right to be treated with dignity, respect, and autonomy throughout the PET-CT imaging process. Healthcare providers should communicate effectively, listen to patients’ concerns, and involve them in decision-making to ensure their preferences and values are respected.
- Access to Results: Patients have the right to access their PET-CT scan results and receive clear explanations from healthcare providers regarding the findings, implications, and recommended next steps. Access to results empowers patients to actively engage in their healthcare management and make informed decisions about treatment options.
- Advocacy and Support: Patients have the right to advocate for their needs and preferences during PET-CT scanning, with the support of family members, caregivers, or patient advocates if desired. Healthcare providers should encourage open communication and collaboration to address patients’ concerns and ensure their well-being throughout the imaging process.
Overall, respecting patient rights and considerations is essential to promoting patient-centered care, enhancing the patient experience, and achieving optimal outcomes in PET-CT imaging. By prioritizing patient safety, comfort, and informed decision-making, healthcare providers can uphold ethical principles and deliver high-quality care that aligns with patients’ needs and preferences.
Privacy and data protection are paramount considerations in PET-CT scanning to safeguard patients’ personal health information and ensure compliance with privacy regulations. Key aspects of privacy and data protection in PET-CT scanning include:
- Confidentiality of Health Information: Patient health information obtained during PET-CT scanning, including medical history, imaging results, and diagnostic reports, is considered sensitive and confidential. Healthcare providers are obligated to maintain the confidentiality of this information and protect it from unauthorized access or disclosure.
- HIPAA Compliance: In the United States, PET-CT facilities must comply with the Health Insurance Portability and Accountability Act (HIPAA), which sets standards for the privacy and security of protected health information (PHI). PET-CT providers must implement HIPAA-compliant practices to safeguard patient privacy and ensure the confidentiality of PHI.
- Consent for Data Sharing: Patients may be asked to provide consent for the sharing of their PET-CT imaging data for research, education, or quality improvement purposes. Healthcare providers must obtain explicit consent from patients before sharing their imaging data with third parties, ensuring transparency and respecting patients’ autonomy.
- Secure Storage and Transmission: PET-CT imaging data should be stored and transmitted securely to prevent unauthorized access or breaches of confidentiality. Healthcare facilities employ secure electronic medical record systems, encryption technologies, and access controls to safeguard imaging data from cyber threats and data breaches.
- Limited Access to Information: Access to PET-CT imaging data and patient health information is restricted to authorized healthcare personnel directly involved in patient care or authorized for legitimate research or administrative purposes. Healthcare providers follow the principle of least privilege, granting access to the minimum amount of information necessary for specific roles or responsibilities.
- Data Retention Policies: PET-CT facilities adhere to data retention policies that govern the storage, retention, and disposal of imaging data and patient health information. These policies ensure compliance with regulatory requirements and minimize the risk of unauthorized access to outdated or unnecessary data.
- Patient Rights: Patients have the right to access their PET-CT imaging data and request amendments or corrections to inaccuracies in their health information. Healthcare providers must facilitate patients’ access to their imaging data and address any concerns or requests related to privacy and data protection.
- Training and Awareness: Healthcare personnel receive training and education on privacy regulations, data protection policies, and best practices for safeguarding patient information during PET-CT scanning. Regular training sessions and awareness programs ensure that staff members understand their responsibilities and uphold privacy standards.
Overall, privacy and data protection measures in PET-CT scanning aim to preserve patient confidentiality, maintain the integrity of health information, and foster trust between patients and healthcare providers. By implementing robust privacy safeguards and adhering to regulatory requirements, PET-CT facilities demonstrate their commitment to protecting patient privacy and ensuring the security of sensitive imaging data.
During the scanning process, patients have certain rights and preferences that should be respected to ensure their safety, comfort, and overall well-being. Some key patient rights and preferences during PET-CT scanning include:
- Informed Consent: Patients have the right to receive clear and comprehensive information about the PET-CT scanning procedure, including its purpose, benefits, potential risks, and alternatives. Informed consent ensures that patients understand the nature of the procedure and can make autonomous decisions about their healthcare.
- Privacy and Dignity: Patients have the right to privacy and dignity during the scanning process. Healthcare providers should ensure that patients are provided with appropriate attire, such as gowns or drapes, to maintain modesty while undergoing the scan. Measures should also be taken to minimize exposure to unnecessary personnel and ensure confidentiality of patient information.
- Comfort and Safety: Patients have the right to feel comfortable and safe during PET-CT scanning. Healthcare providers should address patients’ concerns and anxieties, provide clear instructions, and offer support throughout the procedure to alleviate discomfort and promote a positive experience.
- Communication and Consent: Patients have the right to communicate their preferences and concerns to healthcare providers during the scanning process. Healthcare providers should obtain informed consent from patients before proceeding with the scan and address any questions or requests for clarification.
- Pain Management: Patients have the right to receive appropriate pain management and sedation if necessary to alleviate discomfort during the scanning process. Healthcare providers should assess patients’ pain levels and administer analgesics or sedatives as needed to ensure their comfort and cooperation during the procedure.
- Respect for Cultural and Religious Beliefs: Patients have the right to have their cultural and religious beliefs respected during PET-CT scanning. Healthcare providers should be sensitive to patients’ cultural practices and religious preferences, accommodating special requests whenever possible to ensure a culturally competent and respectful environment.
- Access to Support Persons: Patients have the right to have a support person, such as a family member or friend, present during PET-CT scanning to provide emotional support and assistance if needed. Healthcare providers should accommodate patients’ requests for support persons, recognizing the importance of emotional support during medical procedures.
- Feedback and Complaints: Patients have the right to provide feedback and raise concerns or complaints about their experience during PET-CT scanning. Healthcare providers should encourage open communication, listen attentively to patients’ feedback, and address any issues or grievances promptly and appropriately.
Overall, respecting patients’ rights and preferences during PET-CT scanning is essential to promoting patient-centered care, enhancing the patient experience, and ensuring that patients feel empowered and respected throughout the imaging process. By prioritizing patient comfort, safety, and communication, healthcare providers can create a supportive and positive environment that facilitates optimal outcomes for patients undergoing PET-CT scanning.
Understanding your health condition and evaluating treatment options are essential steps in managing your overall well-being and making informed decisions about your healthcare. Here are some key aspects to consider:
- Education and Information: Take the time to educate yourself about your health condition, including its causes, symptoms, potential complications, and available treatment options. Seek reliable sources of information, such as reputable medical websites, peer-reviewed journals, and healthcare professionals, to gain a better understanding of your condition.
- Consultation with Healthcare Providers: Schedule appointments with healthcare providers, such as primary care physicians, specialists, or surgeons, to discuss your health condition and treatment options. Ask questions, express your concerns, and seek clarification about any aspects of your condition or recommended treatments that you do not understand.
- Diagnostic Tests and Imaging Studies: Depending on your health condition, your healthcare provider may recommend diagnostic tests, such as blood tests, imaging studies (e.g., X-rays, MRI, CT scans), or biopsies, to gather more information about your condition and determine the most appropriate treatment approach.
- Treatment Goals and Preferences: Consider your treatment goals and preferences when evaluating treatment options. Discuss your priorities, values, and preferences with your healthcare provider to ensure that the recommended treatment aligns with your individual needs and preferences.
- Risks and Benefits of Treatment: Understand the potential risks and benefits of each treatment option, including possible side effects, complications, and long-term outcomes. Ask your healthcare provider to explain the anticipated benefits of treatment and any potential risks or adverse effects associated with each option.
- Alternative and Complementary Therapies: In addition to conventional medical treatments, explore alternative and complementary therapies that may complement your treatment plan and support your overall well-being. Discuss these options with your healthcare provider to ensure they are safe and appropriate for your specific health condition.
- Second Opinion: Consider seeking a second opinion from another healthcare provider or specialist to confirm the diagnosis, explore alternative treatment options, or gain additional insights into your health condition. A second opinion can provide valuable perspective and help you make a well-informed decision about your healthcare.
- Shared Decision-Making: Engage in shared decision-making with your healthcare provider to collaboratively discuss and evaluate treatment options based on your individual preferences, values, and goals. Participate actively in the decision-making process by asking questions, voicing your concerns, and expressing your preferences.
- Follow-Up and Monitoring: Once a treatment plan is established, adhere to follow-up appointments and monitoring recommendations outlined by your healthcare provider. Regular follow-up visits and monitoring tests are essential for assessing treatment effectiveness, managing side effects, and adjusting the treatment plan as needed.
By taking an active role in understanding your health condition and evaluating treatment options, you can make informed decisions about your healthcare and actively participate in managing your overall well-being. Remember to communicate openly with your healthcare provider, ask questions, and advocate for your needs to ensure that your treatment plan aligns with your individual preferences and goals.
Collaboration between patients and doctors during the treatment process is essential for achieving optimal health outcomes and ensuring patient-centered care. Here are some key aspects of collaboration between patients and doctors:
- Open Communication: Effective collaboration begins with open and honest communication between patients and doctors. Patients should feel comfortable expressing their concerns, asking questions, and sharing their preferences with their doctors. Similarly, doctors should actively listen to patients, provide clear explanations, and address any questions or concerns raised by patients.
- Shared Decision-Making: Collaboration involves shared decision-making, where patients and doctors work together to develop a treatment plan that aligns with the patient’s preferences, values, and goals. Doctors should present treatment options, discuss the risks and benefits of each option, and involve patients in the decision-making process. Patients, in turn, should actively participate in decision-making by asking questions, expressing their preferences, and voicing their concerns.
- Respect for Patient Autonomy: Collaboration respects the autonomy and preferences of patients, allowing them to make informed decisions about their healthcare. Doctors should respect patients’ rights to make decisions about their treatment, including the right to refuse or request specific treatments based on their personal values and beliefs. Patients, in turn, should be actively engaged in their care and take responsibility for their health decisions.
- Shared Understanding of Treatment Goals: Collaboration involves establishing a shared understanding of treatment goals between patients and doctors. Patients should clearly communicate their treatment goals, preferences, and priorities to their doctors, while doctors should help patients understand the expected outcomes of different treatment options and how they align with the patient’s goals.
- Regular Follow-Up and Monitoring: Collaboration extends beyond the initial treatment decision to include ongoing follow-up and monitoring of treatment outcomes. Patients and doctors should collaborate on developing a follow-up plan, including scheduled appointments, monitoring tests, and assessments of treatment effectiveness. Regular communication and feedback during follow-up visits help adjust the treatment plan as needed and address any concerns or challenges that arise.
- Empowerment and Education: Collaboration empowers patients to actively participate in their healthcare by providing them with the information and resources they need to make informed decisions. Doctors should educate patients about their health condition, treatment options, and self-management strategies, empowering them to take an active role in their care. Patients, in turn, should seek out reliable information, ask questions, and advocate for their needs to ensure they are well-informed and engaged in their healthcare.
Overall, collaboration between patients and doctors fosters a partnership-based approach to healthcare delivery, where patients are actively involved in decision-making, and doctors provide personalized, patient-centered care that respects the autonomy, preferences, and goals of each individual patient. By working together as partners in care, patients and doctors can achieve better health outcomes and improve the overall patient experience.
Frequently Asked Questions

Get a Free Second Opinion
Experienced Burtom Medical Team is Ready to Help

I consent to Burtom Health Group using my aforesaid personal data for the purposes described in this notice and understand that I can withdraw my consent at any time by sending a request to info@burtom.com.